Here are links to additional posts on HIV
- HIV Review Study Notes
Posted on February 28, 2019 by Tom Wade MD - “#121 HIV Care for the Internist” – Help From The Curbsiders
Posted on November 29, 2018 by Tom Wade MD - #41 PrEP For HIV Prevention- Help From The Curbsiders
Posted on November 29, 2018 by Tom Wade MD - Who Should I Test For Silent HIV Infection? Everyone! And Here’s Why – Help From The Curbsiders
Posted on October 25, 2018 by admin - Prognosis of HIV Disease Based On Hospice Admission Criteria
Posted on April 5, 2018 by Tom Wade MD
In this post I link to and excerpts from The Cribsiders‘ #25: HIV for the Pediatrician
MAY 12, 2021 By DR JUSTIN BERK.
All that follows is from the above resource.
GET PREPPED TO DIAGNOSE AND COUNSEL FAMILIES WITH HIV
Pediatric HIV Infection Pearls
- Data from the pre-HAART era demonstrates that children with HIV infection have a high risk of mortality; treatment should be initiated as soon as the diagnosis is made.
- There are significant positive impacts of disclosure of their HIV status to a child with HIV infection (lower rates of depression and improved engagement and adherence in care and to medications).
- PrEP prescription is not restricted to subspecialists — increasing the number of primary care providers who prescribe PrEP is important to address disparities in HIV acquisition.
What is Human Immunodeficiency Virus?
HIV is a virus that impacts your immune system, and if left unabated (untreated without antiretroviral therapy) can over time lead to destruction of your CD4 tells, which makes you vulnerable to AIDS-defining illnesses.
Examples of AIDS-defining illnesses include Pneumocystis jirovecii pneumonia and certain cancers like Burkitt and CNS lymphomas. See the full list of AIDS-defining conditions here.
Rather than using the 1993 CDC clinical and laboratory categories of HIV or the 2014 revised case definition that defines stages of HIV infection, Dr. Agwu rather just thinks about if the patient is on antiretroviral treatment (ART) or not, if their viral load is controlled or not, and if their CD4 count is above 500 or not. Otherwise the categories or stages can feel limiting.
Pediatric HIV Infection
The first case series of pediatric HIV infection was published by the CDC in 1982; by the time this case series was published, most of these infants had already died.
Based on the Children with HIV Early Antiretroviral Therapy (CHER) trial, we know that the earlier you get kids on treatment, the better.
We know that the CD4 count can falsely reassure you in children, because it is higher in general in kids; be concerned for immunocompromise even at higher CD4 counts.
We use trimethoprim-sulfamethoxazole early to prevent PCP pneumonia in children with HIV infection and they should remain on it for the first year of life regardless of CD4 count.
Before we were treating everyone with HIV with ART as soon as possible after diagnosis, we were treating children, because we knew their risk of death was very high.
Once children have survived to age 5, we think that they have some degree of resiliency, but over time they do develop AIDS-defining illnesses. We know from early surveillance data (see this paper published in Pediatrics in 1987) that there can be a significant period of time between acquiring HIV (even perinatally) and becoming symptomatic.
Important to maintain a high index of suspicion for HIV even with older children who present with unusual infections.
Vertical Transmission and Neonatal Infection
In the case of a mom with undetectable viral load who continues on ART during pregnancy, the risk of infection of the newborn is <1%, probably almost zero.
In the case of a mom diagnosed with HIV during pregnancy, there is a period of time during gestation where she is viremic. It is possible for in utero infection to have occurred even if she starts on ART and achieves an undetectable VL during pregnancy. Risk if highest if she acquired the infection during pregnancy, because viremia is so high during acute infection.
If mom was not on ART during pregnancy and diagnosed only peri-partum, risk is 25-40%. With intrapartum AZT for mom, baby’s risk of HIV acquisition decreases to 13%.
Overall, the earlier therapy is started during pregnancy and the more the VL is suppressed, the better. This is why first and third trimester HIV testing is standard of care for routine pregnancy care.
Improvements of vertical transmission rates likely due to increased uptake of HIV testing (though there are disparities in access to testing across populations), better care and early ART for patients with HIV infection, and targeted strategies for PMCT (prevention of mother-to-child transmission):
- intrapartum AZT for mom
- for infants born to a mom with undetectable VL on ART: neonatal prophylaxis for the baby (zidovudine or ZDV, also known as azidothymidine or AZT)
- for infants at higher risk: a three drug regimen (like AZT + 3TC [Lamivudine] + NVP [Nevirapine])
- C-section can also help decrease risk of vertical transmission for a mom with viremia. See the DHHS perinatal HIV guidelines for more!
Neonatal testing regimen for infants who were exposed to maternal HIV:
- Antibody testing of an infant will be positive in the first six months of life due to maternal transmission of antibodies. Must do PCR testing for viral nucleic acids (DNA or RNA PCR)
- Timing of PCR testing: at birth, again at 2 weeks of life, again at 1-2 months of age, and again at 4-6 months of age. Dr. Agwu likes to repeat antibody testing at 18 months of age to confirm that a child has sero-reverted as expected after maternal antibodies have gone away
- If a child has missed testing at one of these recommended time points, Dr. Agwu recommends continuing ART until the next test result has returned.
Breastfeeding if mom is HIV+
Guidelines recommend that mothers in developed countries not breast feed, and that mothers in developing countries exclusively breast feed.
Mixed feeding (alternating between breast milk and formula) in developing countries actually increases the risk of HIV acquisition in babies.
In developed countries, if mom chooses to breastfeed, in the spirit of harm reduction we can support them. For example, it can be an issue of a woman’s safety if she comes from a culture where breastfeeding is expected, because choosing not to breastfeed could indicate to others that something is “wrong” with them.
Dr. Agwu’s practice has supported about 12 HIV+ moms over the past 3 years to breastfeed successfully without any cases of HIV acquisition in the baby. In her practice, the infants stay on six weeks of treatment dose ART, and then daily nevirapine for the duration of breastfeeding. Mom must continue on ART. Serum HIV PCR testing of the infant must be extended out to be after the cessation of breastfeeding.
Dr. Agwu’s practice has seen decreased rates of postpartum depression in their patients who wish to breastfeed and are supported to do so.
The topic of not recommending breastfeeding is being re-examined more in the era of U=U (undetectable = untransmittable).
New HIV diagnosis
When communicating a neonatal HIV diagnosis, recognize that you are walking into a scenario where there are many misconceived notions of what the diagnosis means. Do more listening than talking. Giving the news in person while sitting down, state the diagnosis, and then listen. Listen, then talk, then listen. Knowing where people are coming for is important. And come back the next day, never assuming they remember anything you told them.
Dr. Agwu ends the family meeting by saying, “Whatever you remember, remember the words your baby will be okay.”
Giving the diagnosis is about in part un-arming the stigma surrounding HIV infection. Important to reassure families that it’s okay to kiss the baby and it’s okay if their poop or pee gets on you. Address family’s fears and normalize taking care of the baby.
For neonatal infection, it’s important to start treatment as soon as possible. Treatment options for neonatal infection have broadened over time, and now we can transition to once a day dosing earlier in life than in the past. Liquid formulations are chosen, two medicines from one class and one medicine from another class. See the DHHS 2020 Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection for more. Adjust dose based on weight and labs.
Care of the pediatric patient with confirmed HIV
It is important to understand the child’s degree of immunosuppression, but in general treat them like any baby with respect to their well child care.
Administer vaccines according to the ACIP schedules, although administration of live vaccines (varicella and MMR) should be deferred for children with CD4 cell percentages <15% (see IDSA HIV primary care guidelines under “special considerations for children”).
Engage the family early around the topic of disclosure to the child of their HIV status. Disclosure or non-disclosure can impact the mental and physical health of children. On average, disclosure of the diagnosis happens around 10 years of age, but this is variable and personalized to the family and the social dynamics.
Dr. Agwu encourages families to disclose the diagnosis as early as possible to the child, because of the positive impacts of disclosure (lower rates of depression and improved engagement and adherence in care and to medications).
ART regimens for school age children who weigh more than 35-40kg are now much simpler and resemble the adult regimens.
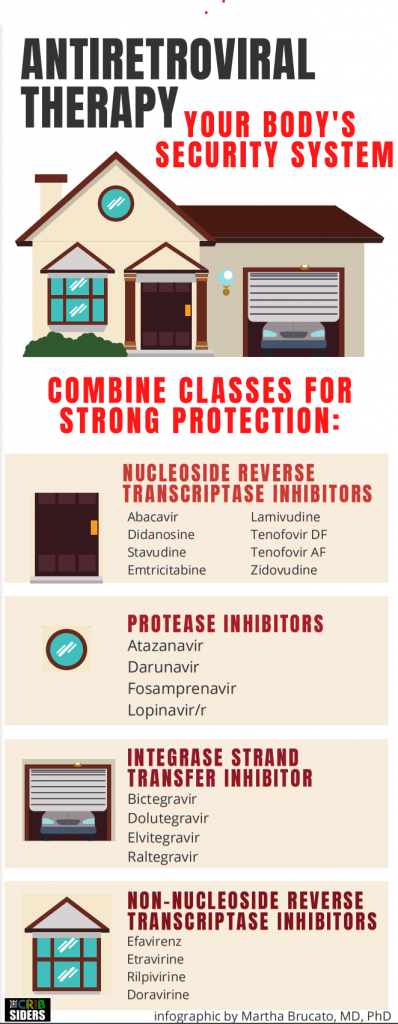
Dr. Agwu explains multi-drug regimens to patients as how to protect their house from a burglar: you have to protect the front door, the window, and the back door.
Acute Retroviral Syndrome
A 16 year old adolescent boy presents to the emergency room with headache, diarrhea, nausea, and diffuse myalgias. Monospot is negative. On social history, the patient discloses that he is sexually active with multiple partners. He estimates he uses condoms 75% of the time.
Acute retroviral syndrome is when you first acquire HIV and there is a rapid increase in your viral load.
The body develops a flu-like illness in response to the infection with lymphadenopathy and systemic inflammation.
We should always have acute retroviral syndrome on our differential (particularly if a patient is within the age range of 13 to 64 years old) if a patient presents with an influenza-like illness. About 60-70% of patients when asked retrospectively at the time of HIV diagnosis can recall a flu-like illness within the prior year.
A note on this diagnosis given the COVID-19 pandemic: be aware of the risk of anchoring or developing tunnel vision on COVID as the final diagnosis, without considering other potential infections (like HIV!), rheumatologic conditions, etc.
How to make the diagnosis of acute retroviral syndrome: with fourth generation HIV testing (combination antigen/antibody tests), the p24 antigen can be detected as early as 7-10 days, so we potentially expect that the fourth generation tests could be positive as early as 7-10 days. However, the sensitivity of the test improves the more time has passed since infection.
Normalize testing so that an HIV test is like any other lab test.
If your suspicion is still high after a negative fourth generation test, Dr. Agwu would recommend sending a serum PCR for HIV DNA or RNA. You could bring a patient back for testing within a week, but Dr. Agwu considers the consequences of a missed diagnosis here (including further transmission).