In this post I link to and excerpt from The Curbsiders‘ [Link is to the episode list] #256 Sarcoidosis [Link is to the podcast and show notes] FEBRUARY 15, 2021 By DEB GORTH:
A GRAND OVERVIEW OF GRANULOMAS WITH DRS. SCHOLAND AND BOLTAX:
Here are excerpts from the show notes:
Sarcoidosis Pearls
- The characteristic noncaseating granulomas of sarcoidosis can be thought of as a callus generated by chronic inflammation, more specifically, antigen driven CD4+ T-cell activation and macrophage recruitment (Patterson et al 2017).
- Pay close attention when patients complain of dyspnea, and workup this complaint with sarcoidosis in your differential.
- Consider sarcoidosis in patients who have received multiple courses of antibiotics for non-resolving pneumonia or upper-respiratory infection.
- About two-thirds of patients who present with bilateral hilar lymphadenopathy will achieve eventual remission, while the remaining third will have chronic disease (Siltzbach et al 1974).
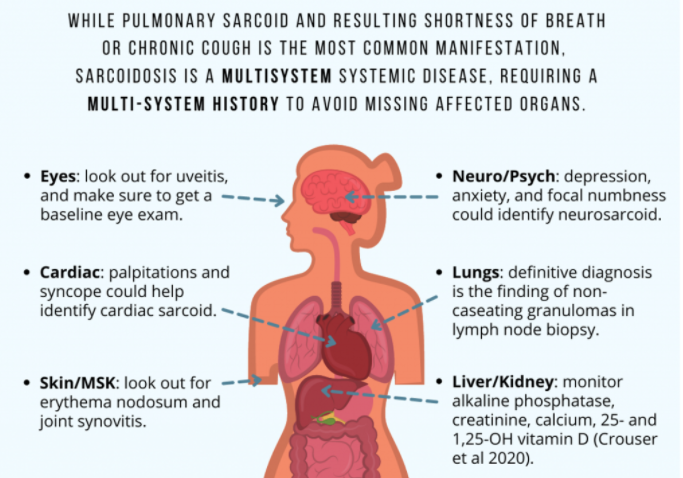
- Sarcoidosis is a multisystem systemic disease, requiring a multi-system history and evaluation to avoid missing affected organs.
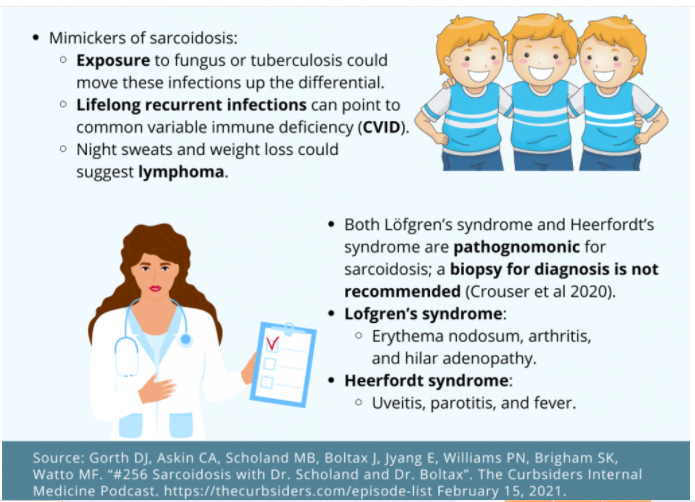
- The central challenge of diagnosing sarcoidosis is ruling out the mimics of this disease: CVID/GLILD, tuberculosis, fungal infection, and lymphoma.
- “The diagnosis of sarcoidosis is arbitrarily made when the statistical likelihood of alternative diagnoses becomes too small to warrant further investigation” (Baugham et al 2010).
- Both Löfgren’s syndrome and Heerfordt’s syndrome are pathognomonic for sarcoidosis; in these instances a biopsy for diagnosis is not recommended (Crouser et al 2020).
- Serum ACE levels have limited diagnostic value for sarcoidosis (Ungprasert et al 2016).
- Additional testing to evaluate systemic involvement should include: baseline eye exam, serum creatinine, alkaline phosphatase, serum calcium, 25- and 1,25-OH vitamin D, and an EKG (Crouser et al 2020).
- There is little correlation between radiographic findings and patients’ sarcoidosis symptoms or functional capacity (Judson et al 2008 and Karetzky and McDonough 1996).
- The cornerstone of therapy for sarcoidosis is glucocorticoids (initial dose prednisone 20-40 mg) (Rahaghi et al 2020).
- If a patient isn’t responding to treatment as expected, even after the diagnosis of sarcoid, reconsider your diagnosis and reinvestigate the other sarcoidosis mimickers before considering second line therapies (biologics/immunosuppressive drugs).
- Sarcoidosis is a high burden disease; this diagnosis has lots of uncertainty regarding progression, requires the care of multiple different providers, and has debilitating symptoms.