Start at 35:00
In this post I link to and excerpt from CoreIM’s Feb 10,2021 show notes and podcast and the transcript of 5 Pearls On Hyponatremia Diagnostics [There is a second episode coming on Hyponatremia Therapeutics].
Here is CoreIM’s link to the excellent and complete article on Hyponatremia from Amboss.
Here are excerpts from the show notes of 5 Pearls On Hyponatremia Diagnostics:
Show Notes
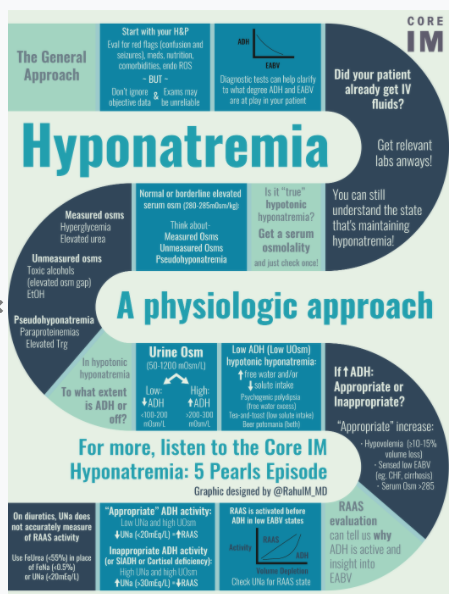
Pearl 1 – General Approach
- Hyponatremia is a significant clinical problem:
- Most common electrolyte disorder, occurring in up to 30% of hospitalized patients
- Mild chronic hyponatremia is associated with more frequent falls – gait and attention impairments have also been observed
- H&P – may be helpful, but don’t ignore other objective data that contradicts!
- History:
- Quickly assess for red flags (confusion, seizures) → immediate intervention, ICU admission
- Ask about dietary history, fluid/EtOH intake, new meds, endocrine ROS, relevant comorbidities
- Physical Examination:
- Volume status is theoretically helpful as diagnostic algorithms hinge on it, but error prone
- Our approach focuses on understanding what each diagnostic test adds vs. rote dependence on algorithm
- More helpful given that most hyponatremia in the hospital is multifactorial
- Ask yourself where your patient with hyponatremia is on “Cartesian space” with:
- Anti-diuretic Hormone (ADH) secretion, as indirectly measured by UOsm relative to
- Effective arterial blood volume (EABV), as estimated based on clinical examination and measurement of urine sodium
- What if we encounter a patient after intervention, and without complete labs or urine studies?
- Still obtain appropriate serum and urine studies as you can assess response to interventions (urine output, change in urine concentration and serum sodium) and the patient’s current ADH/EABV state
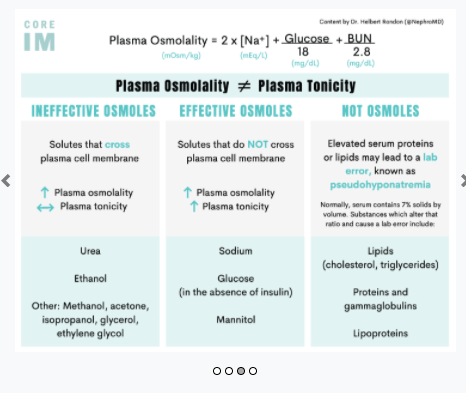
Pearl 2 – Serum Osmolality (Normal value 280-285 mOsm/kg)
- We expect patients with true hyponatremia to have a low osmolality (<280 mOsm/kg)
- This makes sense because sodium is the most significant contributor to osmolality
- SOsm= 2 [Na+] + [Glu]/18 + [BUN]/2.8
- The equation in countries that use the metric system also entails sodium x 2
- Serum osmolality can be thought of as a “quality check” to rule out other osmoles that may be contributing to the hyponatremia.
- If osmolality is normal assess if the patient has high triglycerides or an extra protein in blood (e.g. Multiple myeloma, recent IVIG administration) Such cases referred to as “pseudohyponatremia” = lab artifact, not of clinical significance.
- Computer expects that aqueous component of blood is 93%, with 7% serum particles
- High serum lipids or extra protein changes this ratio and impact the sodium calculation
- Want to be sure? Whole blood sample of serum osmolality will not be subject to this error
- Such cases referred to as “pseudohyponatremia” – laboratory artifact
- If osmolality is elevated (usually >280-285 mOsm/kg), or if normal osmolality without elevated proteins/lipids, look for extra osmoles, either measured or unmeasured!
- Measured: Severe hyperglycemia, BUN
- Unmeasured: ETOH, Toxic alcohols, iodinated contrast, sucrose
- Serum osmolality assessment prompts us to consider effective and ineffective osmoles at play:
- Effective osmoles (sodium, glucose, potassium) do not cross the plasma membrane, and therefore cause shifts in water movement (impact tonicity)
- Most of the clinical complications that arise as a result of hyponatremia (and its correction) are driven by the fact that sodium is an effective osmole – it impacts tonicity, and therefore cell size.
- Ineffective osmoles (ethanol, urea, lactate) cross the plasma membrane more readily, and therefore do not cause shifts in water movement (does not change tonicity)
- Serum osmolality is not a serially measured lab!
- Measure it once unless there is a significant sodium change that is difficult to contextualize.
And here are the infographics summarizing the podcast and show notes:
Text
Text
Text