In this post, I link to and excerpt from The Curbsiders‘ [link to the complete episode list] #279 Dominate Stable Angina with the CardioNerds. JUNE 14, 2021 By DR. MOLLY HEUBLEIN.
All that follows is from the above podcast and show notes:
We deconstruct it’s pathophysiology, diagnosis, and management with Drs. Dan Ambinder and Rick Ferraro. Topics: When to order coronary CT vs Stress testing; An approach to non-obstructive coronary disease; What treatments are life prolonging; Medical therapy vs Stenting; An approach to antianginal therapy; and how to partner with each patient. Listen as we dive deep into the recent literature and recommendations to dominate stable angina.
Stable Angina Pearls
- Stable angina and unstable angina/ACS have inherently different pathophysiologies. The plaque blockages in stable angina are hard and fixed, so the disease does not tend to change acutely. In ACS, patients have sudden plaque rupture with coagulation, inflammation, and acute blood flow limitation leading to infarction.
- Anatomical testing (coronary catheterization, CT angiography) will show you what the coronary tree looks like. Functional (stress) testing will show you what the muscle is feeling based on the blood flow.
- Multiple trials, including the recent ISCHEMIA trial, have shown that in patients with stable ischemia, angioplasty (stenting) does not have a mortality benefit when added to optimal medical therapy (when compared to medical therapy alone).
- Goals of treatment for stable angina include improving longevity (blood pressure control, statins, aspirin) and improving symptoms (beta-blockers, ranolazine, stenting).
Stable Angina
Definitions
Stable angina is defined as chest pain or equivalent symptoms (such as chest discomfort or dyspnea) that occur predictably with exertion and are relieved with rest. The pathophysiologic foundation is supply-demand mismatch. During times of rest, there is adequate blood flow to sustain the myocardium. During times of stress ( i.e. exercise), flow limitation causes myocardial ischemia which can manifest as pain, dyspnea, nausea, or other symptoms.
Unstable angina is diagnosed when those same types of symptoms arise with a lower amount of exercise. Presently, this is a less common diagnosis in the era of high-sensitivity troponin testing which has resulted in more cases of unstable angina being more appropriately diagnosed as NSTEMI (non-ST-elevation myocardial infarction).
The pathophysiology is inherently different. In stable angina, the plaque is a fixed obstruction. The plaque is “stable” due to it being calcified and hard. With unstable angina and NSTEMI/STEMI, there is an acute plaque rupture or endothelial erosion. It is a dynamic process with platelet activation and ongoing thrombosis. As such, symptoms can acutely change.
Risk Factor Assessment
When assessing symptoms of chest pain, it’s important to consider the patient’s risk factors, and view their history through the lens of these known risk factors. The more risk factors, the higher the pre-test probability. That said, there are outliers! Certainly young patients can experience ACS, and women classically can present with ACS without the traditional symptomatology so it is important to take a presentation of chest pain syndrome seriously and consider CAD (ECS 2019 Guidelines).
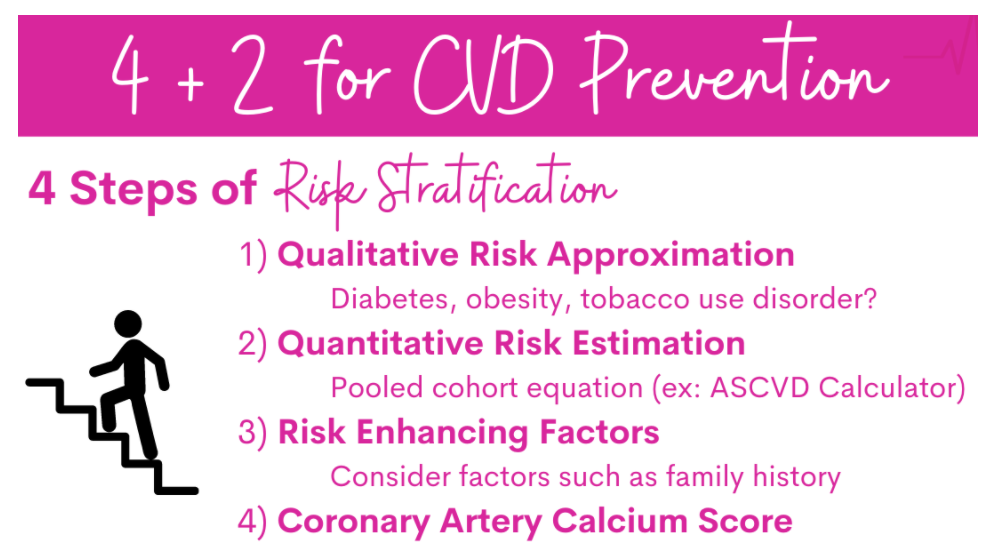
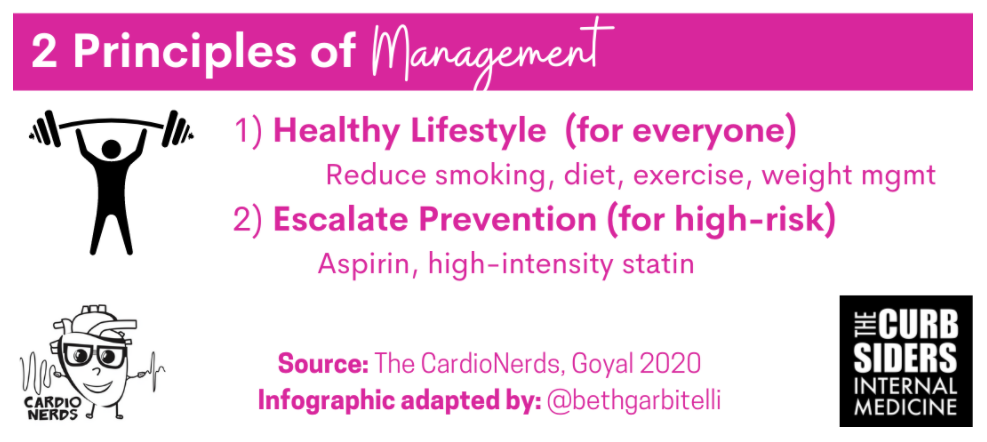
4+2 for CVD prevention (Goyal 2020)
- Qualitative risk assessment: Does the patient have diabetes, obesity, tobacco use disorder?
- Quantitative risk assessment: Pooled cohort equation like the ASCVD Risk Calculator
- Risk enhancing factors: Consider things that are poorly represented in the risk calculators, like family history.
- Consider checking a coronary artery calcium score (CAC score).
Take these together and assess overall risk. Then the +2 is treatment:
- Healthy lifestyle
- Escalate preventative measures for patients at higher risk- aspirin, high intensity statin
- High intensity statins: atorvastatin 40–80 mg, rosuvastatin 20–40 mg, or (less commonly) simvastatin at 80 mg (Yu 2020)
There is much more in the show notes and they should be reviewed in their entirety.