In this post, I link to and excerpt from The Curbsiders‘ #316 Lower Extremity Edema with The Curbsiders.
JANUARY 17, 2022 By Dr PAUL WILLIAMS
All that follows is from the above resource.
We have seen our esteemed guests, and they are us! Paul Williams (@PaulNWilliamz) leads the discussion with Matt Watto (@DoctorWatto) and Beth “Garbs” Garbitelli (@bethgarbitelli) on the evaluation and management of common causes of edema.
Edema Pearls
- The pathophysiology behind edema is an imbalance between oncotic pressure and hydrostatic pressure within the venous system.
- Chronic venous insufficiency* is the most common cause of chronic lower extremity edema, especially in older patients.
- *Venous Insufficiency
Updated: Sep 25, 2020
Author: Robert Weiss, MD from emedicine.medscape.com- Again, bilateral lower extremity cellulitis is extremely uncommon.
- Edema may be a sign cardiopulmonary, renal, hepatic, or thyroid dysfunction – so look at the patient in front of you and evaluate for risk factors.
- Lymphedema results from impairment of lymphatic return, and can sometimes be distinguished from other causes of edema by the Stemmer sign.
- Medications are a common cause of lower extremity edema – don’t forget about the gabapentinoids!
- May-Thurner syndrome is caused by anatomical compression of the left iliac vein, and can result in unilateral edema or recurrent deep vein thrombosis.
- Acute edema can be caused by deep vein thrombosis, cellulitis, or ruptured popliteal cyst, all of which may be difficult to differentiate from each other.
- The physical examination should be directed at finding underlying systemic causes of lower extremity edema.
- Management of edema usually includes compression, elevation, and avoidance of exacerbating medications.
Lower Extremity Edema Notes
Edema – Pathophysiology
Generally speaking, venous circulation maintains a balance between hydrostatic pressure and oncotic pressure. Edema can result from perturbations in these forces (Trayes et al 2013).
- Increased hydrostatic pressure
- Venous hypertension from right-sided heart failure, venous insufficiency, constrictive pericarditis, etc.
- Endoluminal obstruction (e.g. venous thrombosis, popliteal cyst, etc.)
- Decreased oncotic pressure
- Low-protein states like nephrotic syndrome, hepatic failure, protein-energy malnutrition
- Capillary dilation
- Vasodilation from warmer weather
- Inflammatory states such as burns or cellulitis
Recall that venous return is largely a passive process and requires functional valves and muscle contraction. Defects in either of these can result in diminished venous return, increased venous pressure, and resultant edema.
Determining the Cause – Chronic Edema
Chronic venous insufficiency
- Ultrasonography from emedicine.medscape.com
- “Duplex ultrasonography is the study of choice for the evaluation of venous insufficiency syndromes.”
- Probably the most common cause (Beebe-Dimmer et al 2005)
- Prevalence increases with age
- More common in patients with obesity
- Represents a spectrum of disease from painless edema to chronic ulcerative disease
- A gentle reminder: bilateral cellulitis of the lower extremities is uncommon
Cardiogenic causes
- Evaluate patients for signs and symptoms of heart failure and untreated or undiagnosed obstructive sleep apnea
Renal causes
- Evaluate for risk factors for nephrotic syndrome
- Don’t forget to look for periorbital edema (and don’t forget Tony Breu’s amazing Tweetorial)
Hepatic causes
- Evaluate for stigmata of chronic liver disease
Thyroidal causes
- Pretibial myxedema (thyroid dermopathy)
- Rare manifestation of Graves’ disease
- Typically bilateral and non-pitting
- Hypothyroidism can also lead to non-pitting edema
Lymphedema
- Can be idiopathic or secondary
- Secondary lymphedema can be caused by surgery or radiation
- Filariasis most common cause worldwide (Green 2015)
- Caused by an impediment of lymphatic return
- Chronic leakage of proteins leads to inflammation and ultimately fibrosis
- Results in thickening of the skin and tissues
Lipedema
- Pathologic accumulation of adipose tissue in the lower extremities
- Classically spares the feet
Medication-induced
- Thiazolidinediones.
- NSAIDs
- Calcium channel blockers
- Dihydropyridines more than non-dihydropyridines
- Effect tends to be dose-dependent
- Edema from calcium channel blockers not effectively treated by diuretics
- Angiotensin-receptor blockers or ACE-inhibitors are more effective at mitigating this
- Gabapentinoids
- Mechanism thought to be due to vasodilatory effects and decreased myogenic tone (Largeau et al 2021)
- Oral contraceptives
- Corticosteroids
May-Thurner syndrome
- Cause of unilateral lower extremity edema
- Female predominant
- Compression of the left iliac vein by the right iliac artery
- Can predispose to left lower extremity DVT
Neuromuscular causes
- Any condition that affects calf muscle strength can lead to edema (Ratchford and Evans 2017)
- Includes stroke, multiple sclerosis, and even lumbar radiculopathy
Determining the Cause – Acute Edema
Deep vein thrombosis
- Likelihood can be predicted by calculating Wells score
- Generally requires ultrasonography for diagnosis
Cellulitis
- Clinically difficult to differentiate from DVT
Ruptured popliteal cyst
- Classically presents with ecchymosis around the ankle
- Again, may be clinically challenging to differentiate from other causes
- Ultrasonography usually required to make the diagnosis
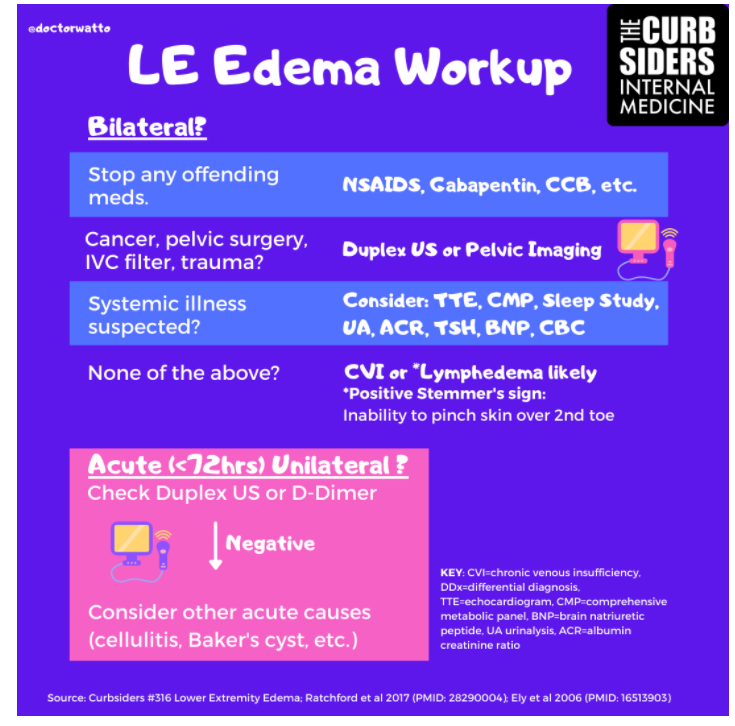
Edema – The Workup
Physical Examination
- Assess for symptoms of cardiac disease
- Assess for JVD
- Pitting edema can be extensive and extend proximally to the sacrum in heart failure
- Evaluate for pitting versus non-pitting
- Non-pitting edema seen in lymphedema
- Check for Stemmer’s sign to evaluate for lymphedema
- Inability to pinch the skin at the base of the toes due to skin changes
- Evaluate for superimposed cellulitis if chronic changes of venous insufficiency are seen
Laboratory evaluation
- Reasonable to check urine protein-creatinine ratio
- In most patients, could consider comprehensive metabolic panel to evaluate albumin and electrolyte abnormalities
- TSH often checked to rule out thyroid causes
- Additional testing, such as urinalysis, complete blood count, BNP, or D-dimer, could be considered depending on patient history and risk factors
Other studies
- Venous ultrasound studies should be ordered if there is suspicion for DVT
- Consider a transthoracic echocardiogram in patients with cardiopulmonary symptoms
- Polysomnography is appropriate for patients for whom there is high suspicion for sleep apnea
- Abdominopelvic imaging may be appropriate when the cause is not fully elucidated and there is suspicion for malignancy or other compressive or obstructive etiology
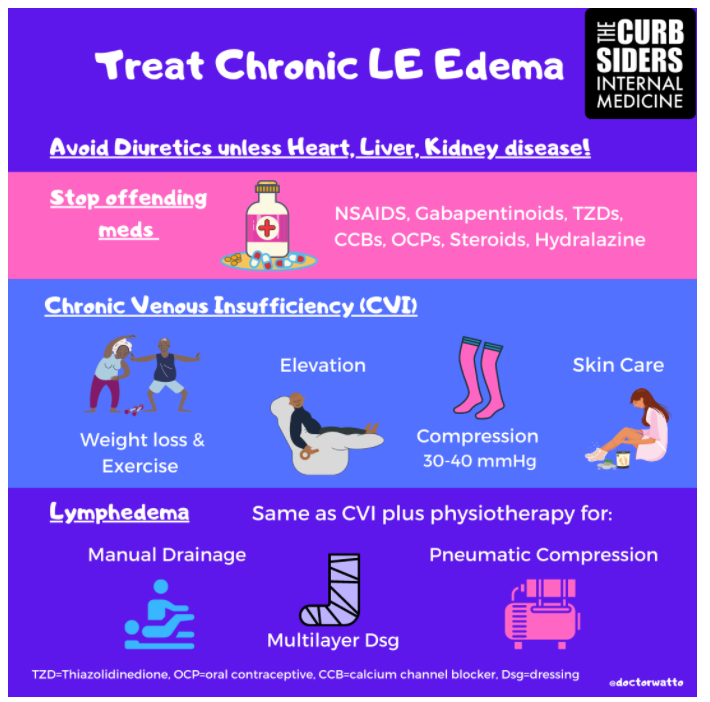
Edema – Management
General principles
- Stop exacerbating medications, if possible
- Compression stockings are generally helpful, especially for chronic venous insufficiency
- Avoid if arterial insufficiency is suspected
- Elevate the legs when possible
- Diuretics may not be helpful in the absence of volume overload
- They are not effective at mitigating edema caused by calcium channel blockers
- Patient education and reassurance are an important component of management
- There is some evidence for horse chestnut seed extract in the short-term treatment of chronic venous insufficiency (Pittler and Ernst 2012)
Lymphedema management
- Best managed by a multidisciplinary team
- Usually includes physical therapy and vascular surgery teams
- Patients typically undergo complex decongestive physiotherapy
- Primary care provider role is to help provide meticulous skin care and ensure care coordination