In this post, after reviewing the chapter, I link to Dr. Farkas’ Internet Book Of Critical Care (IBCC) [Link is to the Table of Contents] – Reversible Cerebral Vasoconstriction Syndrome (RCVS), June 14, 2021 by Josh Farkas.
All that follows is from the chapter.
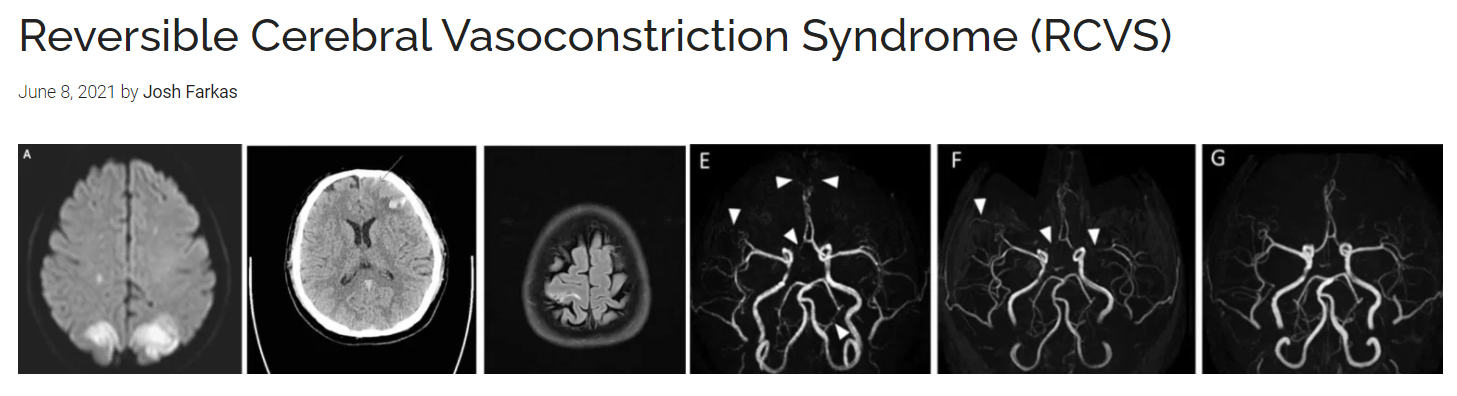
Reversible Cerebral Vasoconstriction Syndrome (RCVS) is an important cause of stroke and intracranial hemorrhage, especially in younger people. This disorder may also complicate other neurologic disorders, especially Posterior Reversible Encephalopathy Syndrome (PRES).
CONTENTS
- Introduction
- Epidemiology
- Clinical features
- Diagnosis
- Management
- Prognosis
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
introduction
basics of Reversible Cerebral Vasoconstriction Syndrome (RCVS)
- RCVS typically presents with thunderclap headache due to diffuse cerebral vasospasm. RCVS is usually benign, but can cause severe sequelae (most notably, ischemic strokes).
- Historically, RCVS has been known as numerous other entities, some of which are listed here:(31272323)
- Thunderclap headache with reversible vasospasm.
- Benign angiopathy of the central nervous system.
- Postpartum angiopathy.
- Migrainous vasospasm, or migraine angiitis.
- Drug-induced cerebral arteritis or angiopathy.
- Sexual headache.
- Call-Fleming syndrome.
- It is only recently that these varied presentations have been unified under the rubric of RCVS. The ability to diagnose vasospasm noninvasively, by using either CT or MR angiography, has dramatically advanced the field. With a clearer concept of RCVS and improved diagnostic tools, it’s likely that RCVS will be diagnosed more often in the future.
pathophysiology
- The primary problem seems to be diffuse, multifocal vasospasm of intracranial arteries. This may start with the smaller distal vessels and progress proximally to the larger arteries.
- The cause isn’t clear, but it may relate to autonomic hyperactivity and/or endothelial dysfunction.(29274685) Histology does not reveal any inflammatory or vasculitic process.
- The pathogenesis of the thunderclap headache is unclear. It’s conceivable that this results from a positive feed-forward cycle involving increasing pain, increasing sympathetic tone, and increasing vasospasm due to innervation of arteries via the first division of the trigeminal nerve.
epidemiology
general epidemiology
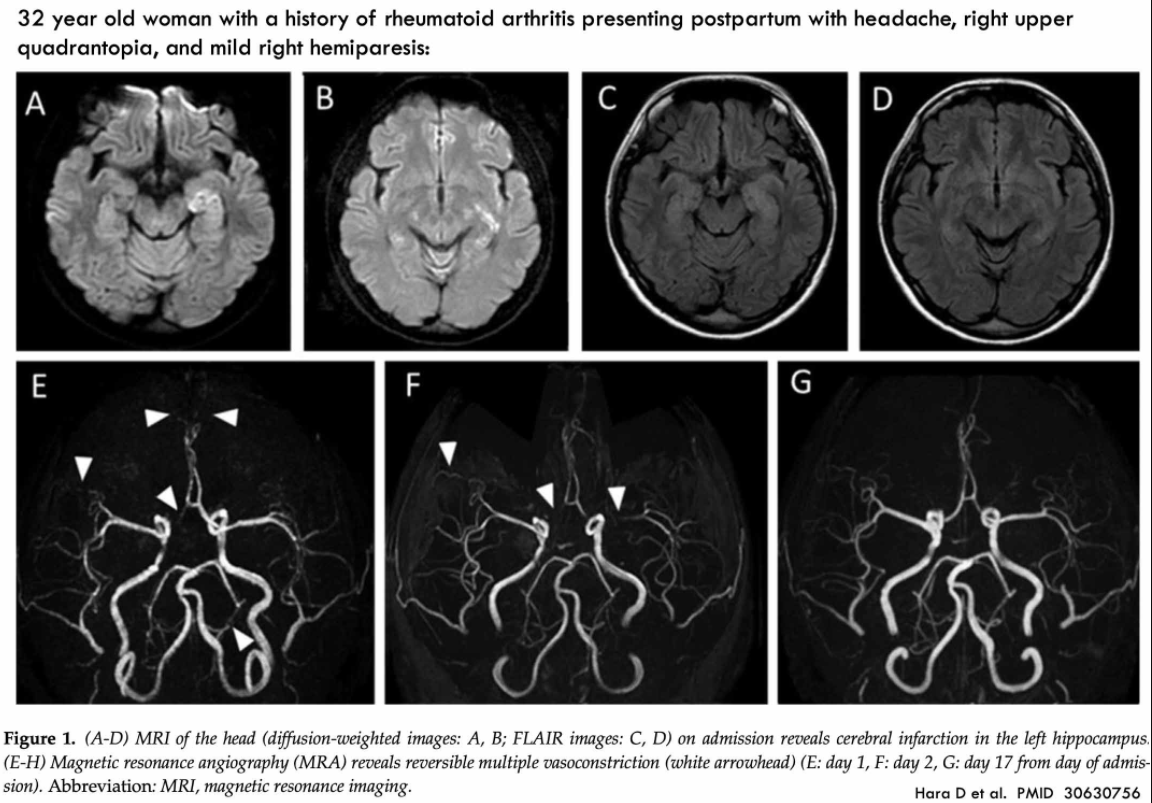
- Women are more commonly affected than men (with ratios ranging from 2:1 to 10:1).
- The average age is ~40 years old. RCVS occurs predominantly between the ages of 20-50, being reported up to 76 years old.(28456915)
- Though relatively uncommon, RCVS is probably more common than previously recognized (due to underdiagnosis). This may be especially true in the ICU, where RCVS may occur as a complication of other neurological conditions (especially PRES).
risk factors & triggers
- Migraine headaches and antimigraine therapies (e.g., triptans).
- Pregnancy, (pre)eclampsia, postpartum (up to six weeks), ovarian stimulation, or oral contraceptive medications.
- Medications:
- Antidepressants (e.g., SSRIs, SNRIs).
- Adrenergic agents:
- Alpha-agonists (e.g., pseudoephedrine, phenylpropanolamine, nasal decongestants).
- Epinephrine.
- Chemotherapeutics (e.g., cyclophosphamide, tacrolimus).
- Illicit substances (e.g., sympathomimetics, marijuana, LSD).
- Blood transfusion, intravenous immune globulin (IVIG).
- NSAIDs. (29274685)
- Hypercalcemia.
- Trauma (head trauma, neurosurgery).
- Secondary complication of another cerebrovascular disease:
- Cerebral venous thrombosis (CVT).
- Carotid or vertebral artery dissection.
- Posterior reversible encephalopathy syndrome (PRES).
- Cerebral Hyperperfusion Syndrome status post carotid endarterectomy.
clinical features
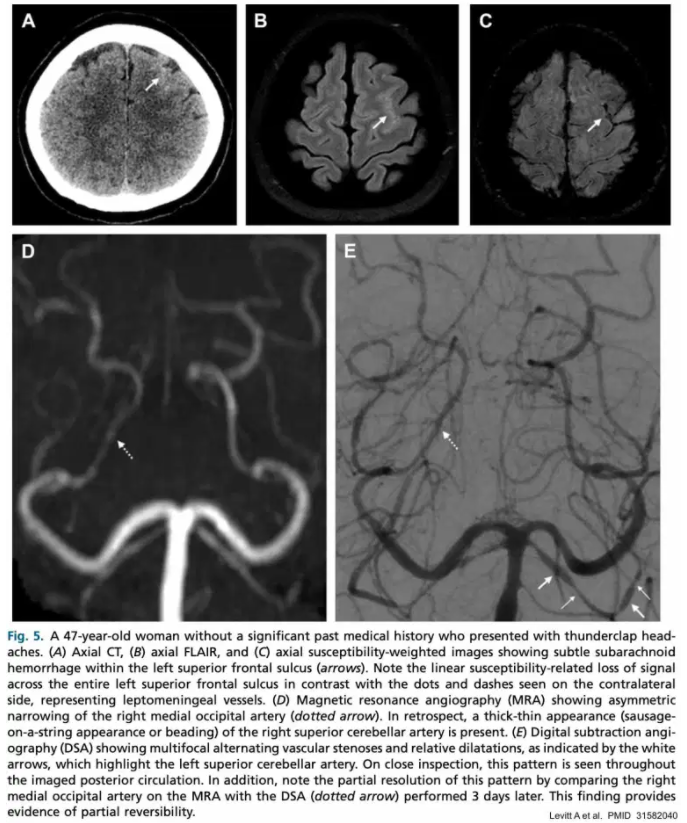
thunderclap headache
- 95% of patients present with a severe headache that reaches maximum intensity within a minute.
- Associated features may include nausea and vomiting, photophobia, phonophobia, and visual changes. Pain may be so severe as to cause screaming and collapse.(29274685)
- Pain often improves within 1-3 hours, which helps differentiate this from subarachnoid hemorrhage.
- Headaches in RCVS tend to recur within days to weeks.(28456915) A history of multiple thunderclap headaches recurring over several days is nearly pathognomonic for the diagnosis of RCVS.
- Headaches may be triggered by exertion, emotion, sex, swimming, bathing/showering, or Valsalva maneuvers (coughing, sneezing, defecation).
- RCVS is the most common cause of true thunderclap headache (pain reaching maximal severity in <1 minute) in patients without aneurysmal subarachnoid hemorrhage.(28456915, 29274685)
- The differential diagnosis of thunderclap headache includes:
- Subarachnoid hemorrhage (SAH).
- Cervical artery dissection.
- Cerebral venous thrombosis (CVT).
- Acute hypertensive emergency.
- Intracerebral hemorrhage.
- Ischemic stroke.
- Some patients may experience a more gradual onset of headache (e.g., over 1-2 hours).
- Some patients don’t present with headache at all, but rather present initially with marked neurologic deficits. It’s possible that some of these patients may have primary PRES complicated by secondary RCVS (more on this here).
subsequent neurological sequelae
- >90% of RCVS patients ultimately have a benign course. However, most patients may experience one of the following neurological sequelae. These typically evolve within 1-2 weeks of the initial headache, as vasospasm continues to intensify. Clinical symptoms will vary widely, depending on which sequelae occur (e.g., ischemic strokes may cause focal neurological deficits). Hemorrhages and seizures usually occur within a week of onset, whereas ischemic complications occur after 2-3 weeks.(29274685)
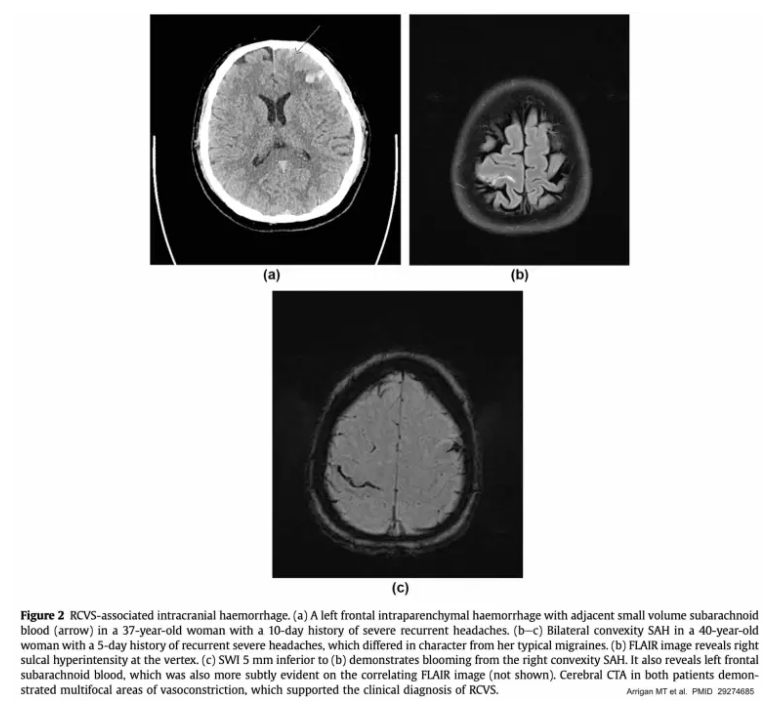
- Intraparenchymal hemorrhages occur in ~10% of patients. These are usually small and lobar.
- Convexity subarachnoid hemorrhage (i.e., subarachnoid hemorrhage occurring on the cortical surface of the brain) occurs in about a third of patients.
- These hemorrhages are typically small and self-limited, located near the vertex of the head.
- In some cases, a convexity SAH provides a key clue which helps reveal the diagnosis of RCVS.
- Seizures (relatively uncommon).
- Ischemic strokes:
- These most often occur in a symmetric distribution along arterial watershed areas, between the anterior and posterior circulation.
- If infarcts are seen within the anterior or posterior cerebral artery territories, this may suggest a concomitant cervical artery dissection which warrants additional investigation.(28456915)
diagnosis
noncontrast CT scan
- CT imaging is often initially normal.
- CT may detect complications of RCVS:
- Hemorrhagic complications may be most notable: lobar intracerebral hemorrhage, convexity subarachnoid hemorrhage, or even subdural hematoma.
- Ischemic infarction.
RCVS is the most common cause of cortical surface (convexity) subarachnoid hemorrhage in patients under 60 years old. More on the differential diagnosis of convexity SAH here.
CT angiography (CTA)
- CT with CTA is often the initial test of choice for RCVS (e.g., patients presenting with thunderclap headache). CT with CTA can be performed emergently, rapidly excluding more dangerous diagnostic possibilities such as aneurysmal subarachnoid hemorrhage. Some centers routinely include CT angiography of the neck as well, given an association between RCVS and cervical neck dissection.(29274685)
- The characteristic finding on CT angiography is smooth, tapered vasoconstriction that is followed by abnormally dilated segments (a “string and beads” pattern). Vasoconstriction is widespread and bilateral. The differential diagnosis of beaded vessels includes vasospasm following subarachnoid hemorrhage, primary angiitis of the central nervous system, and intracranial atherosclerosis.(29274685)
- CT angiography has a sensitivity of 80% when compared to invasive angiography (the gold standard, which is rarely used as a first-line diagnostic tool in clinical practice).(31272323) CT angiography may be normal at the time of initial presentation, only revealing vasoconstriction >3-5 days later. Vasoconstriction is often maximal about two weeks after the initial symptoms.(29274685)
MRI
- Similar to noncontrast CT scanning, about half of MRI scans may be normal initially.(28456915)
- MRI may show vasogenic edema and/or FLAIR hyperintensity that is symmetrically distributed in a watershed distribution.
- Hyperintense vessels (“dot sign”) on FLAIR imaging may be caused by slow blood flow through small blood vessels.(31272323)
- This is seen in ~20% of patients with RCVS.
- Hyperintense vessels correlate with impaired blood flow and development of clinical complications (PRES and ischemic stroke).
- This may be a very early finding, which is observed before spasm of the larger vessels becomes evident on angiography.(31272323)
- The differential diagnosis of the “dot sign” includes leptomeningeal carcinomatosis, meningitis, and status epilepticus.(29274685)
MR angiography (MRA)
- MR angiography (MRA) has a similar performance compared to CT angiography, with a sensitivity of ~80% compared to invasive angiography.(31272323)
- MRA may have the added benefit of evaluating for cervical artery dissection, which may occur simultaneously with RCVS. However, this requires specifically ordering a cervical MRA and protocoling the study appropriately. Cervical MRA may often require intravenous contrast, unlike an isolated MRA of the brain (which may often be done without intravenous contrast, by using time-of-flight MRI techniques to detect flowing blood).
digital subtraction angiography (invasive angiography)
- Invasive angiography is the gold standard diagnostic test, but it is less commonly used in clinical practice. In the context of RCVS, angiography may carry a 9% risk of provoking ischemia.(29274685)
- It is generally unnecessary to immediately reach diagnostic certainty regarding RCVS (because >90% of patients will improve spontaneously and because there are no proven therapies for RCVS). Thus, it may be safer to tolerate some diagnostic uncertainty and perform a repeat CTA or MRA (rather than proceeding immediately to invasive angiography).
- Invasive angiography may offer the ability to perform angioplasty or local administration of vasodilators. However, neither of these therapies is proven to cause clinical improvement. Excess vasodilation could theoretically increase the risk of hemorrhagic transformation.
- In the case of diagnostic uncertainty, a blood vessel’s response to intra-arterial vasodilator infusion supports the diagnosis of RCVS as opposed to primary CNS angiitis (which will not respond to this therapy).
- Indications for invasive angiography might include:
- (1) Progressive clinical deterioration despite conservative management.
- (2) Inability to exclude aneurysmal subarachnoid hemorrhage.
- (3) Persistent diagnostic uncertainty.
lumbar puncture
- Lumbar puncture is generally normal in RCVS, but this may be required to exclude alternative diagnoses.
- Although RCVS can cause small subarachnoid hemorrhages along the cortical surface, RCVS doesn’t cause the lumbar puncture findings which are seen in aneurysmal subarachnoid hemorrhage (e.g., xanthochromia and elevated erythrocytes).
management
possible indications for ICU admission
- Observation in patients with severe angiographic abnormalities.
- Patients with focal ischemic strokes, intracranial hemorrhages, or seizure.
>90% of patients will improve spontaneously, so conservative therapy is appropriate for nearly all patients.
analgesia
- Opioid analgesia may be required. If so, an aggressive bowel regimen should be used to avoid constipation (which may lead to Valsalva maneuvers, which can worsen RCVS).
- Adjunctive acetaminophen may be beneficial.
- NSAIDs may be undesirable in the context of a risk of intracranial hemorrhage. Furthermore, NSAIDs have been implicated in causing RCVS.(28456915)
blood pressure management
- There is no high-quality data regarding optimal blood pressure management.
- Hypotension:
- Probably detrimental.
- Management should involve ensuring a state of euvolemia.
- Note that vasopressors could exacerbate RCVS – so these may not be desirable.
- Hypertension:
- If severe, treatment may be considered.
- Ensure that pain is adequately treated, as this may be a contributing factor to hypertension.
- Nimodipine or a calcium channel blocker might be the agent of choice, given some possibility that this may improve vasospasm of the smaller vessels.
vasodilators
- No high-quality data exists, which does not allow any strong recommendations to be made.
- Some reported cases suggest a benefit from 2-4 grams of IV magnesium sulfate, which may be reasonable (especially among patients with low magnesium levels).(27366294) This can be followed by oral magnesium as a maintenance therapy.
- Nimodipine was not found to improve vasospasm in two prospective case series. Given that hypotension could aggravate brain perfusion, the value of nimodipine is not clearly defined (aside from patients with severe hypertension who need an antihypertensive medication). However, calcium channel blockers such as nimodipine and verapamil are routinely used in many centers in an effort to relieve vasoconstriction. These are generally discontinued once symptoms improve, although some centers continue their use for up to 30 days.
- Intra-arterial vasodilation and angioplasty by neurointerventional radiology may be considered in severe and progressive cases.
seizure management
- Seizures should be treated as per usual regimens (e.g., see the chapter on status epilepticus).
- Seizure prophylaxis isn’t indicated.
prognosis
- Most patients will do well. Cerebral vasoconstriction will resolve over time (hence the name reversible cerebral vasoconstriction syndrome). Unfortunately, parenchymal damage due to ischemia or hemorrhage may not always resolve.
- Progressive vasoconstriction can occur in <5% of patients (leading to large ischemic strokes). This may be more common among postpartum women.
- Following resolution, recurrent RCVS is very uncommon.
Pitfalls
- Beware of misdiagnosing RCVS as a migraine headache, because some of the treatments for migraine (particularly triptans) may exacerbate RCVS.
- RCVS may coexist with cervical artery dissection, so patients with RCVS and neck pain require further evaluation for cervical artery dissection.(28456915)*
*MR angiography (MRA) [How to do Imaging Evaluation for Cervical Artery Dissection. This section is from an earlier part of the chapter.]
- MR angiography (MRA) has a similar performance compared to CT angiography, with a sensitivity of ~80% compared to invasive angiography.(31272323)
- MRA may have the added benefit of evaluating for cervical artery dissection, which may occur simultaneously with RCVS. However, this requires specifically ordering a cervical MRA and protocoling the study appropriately. Cervical MRA may often require intravenous contrast, unlike an isolated MRA of the brain (which may often be done without intravenous contrast, by using time-of-flight MRI techniques to detect flowing blood).
The Internet Book of Critical Care is an online textbook written by Josh Farkas (@PulmCrit), an associate professor of Pulmonary and Critical Care Medicine at the University of Vermont.