In this post, I link to CDC Resources On HIV Diagnosis, Treatment, And Prevention.
HIV Nexus CDC Resources For Clinicians
Effective HIV prevention and treatment occurs across a continuum of care. This comprehensive approach spanning from HIV screening to treatment can help reduce new HIV infections and improve health outcomes among people with HIV (PWH). The CDC HIV Nexus is a one-stop location for information across the HIV continuum, including up-to-date tools and guidelines for your practice, and educational materials for your patients.
HIV screening is recommended for all adolescents and adults 13-64 years of age. Testing can reduce HIV transmission and early diagnosis can improve medical outcomes.
Benefits of Routine Screening
HIV Testing. Linkage to Care. The Time Is Now.
An estimated 1.1 million people in the United States have the human immunodeficiency virus (HIV), and approximately 1 in 7 (nearly 15%) are unaware of their status. About 40% of new HIV infections are transmitted by people undiagnosed and unaware they have HIV.Diagnosing HIV quickly and linking people to treatment immediately are crucial to achieving further reduction in new HIV infections.1
Primary care providers (PCPs) are the front line for detecting and preventing the spread of HIV. The Centers for Disease Control and Prevention (CDC) is asking PCPs to2:
- Conduct routine HIV screening at least once for all their patients
- Conduct more frequent screenings for patients at greater risk for HIV
- Link all patients who test positive for HIV to medical treatment, care, and prevention services
Missed Opportunities for HIV Testing
Despite seeing a PCP, many people at high risk* for HIV are not getting tested every year.4 More than 75% of patients at high risk for HIV who saw a PCP in the last year weren’t offered an HIV test4 during their visit.
*Persons likely to be at high risk include: PWID and their sex partners, persons who exchange sex for money or drugs, sex partners of persons with HIV infection, and MSM or heterosexual persons who themselves or whose sex partners have had more than one sex partner since their most recent HIV test.
Learn more about benefits of early ART and HIV Treatment and Care.
Benefits of Early HIV Diagnosis
People with HIV who are aware of their status should be prescribed ART and, by achieving and maintaining an undetectable (<200 copies/mL) viral load, can remain healthy for many years.5 ART is now recommended for all people with HIV, regardless of CD4 count.6 Studies show that the sooner people start treatment after diagnosis, the more they benefit from ART. Early diagnosis followed by prompt
ART initiation5,7:
- Reduces HIV-associated morbidity and mortality
- Greatly decreases HIV transmission to others
- May reduce risk of serious non-AIDS‒related diseases
Learn more about undetectable viral load and effectively no risk of transmission.
How Often Should Patients be Screened?
The CDC recommends that individuals between the ages of 13 to 64 get tested for HIV at least once as part of routine health care and that those with risk factors get tested more frequently. Patients who may be at high risk for HIV should be screened at least annually 2, 9:
- PWID and their sex partners
- People who exchange sex for money or drugs
- Sex partners of people with HIV
- Sexually active MSM (more frequent testing may be beneficial; e.g., every 3‒6 months)
- Heterosexuals who themselves or whose sex partners have had ≥1 sex partner since their most recent HIV test
- People receiving treatment for hepatitis, tuberculosis, or a sexually transmitted disease
Routine HIV Screening is endorsed by:
Newer, Improved HIV Tests Allow for Earlier HIV Detection
HIV tests have improved substantially over the years, and are now easier and less expensive, with a more rapid turnaround time for results.1
Three types of HIV tests are available:
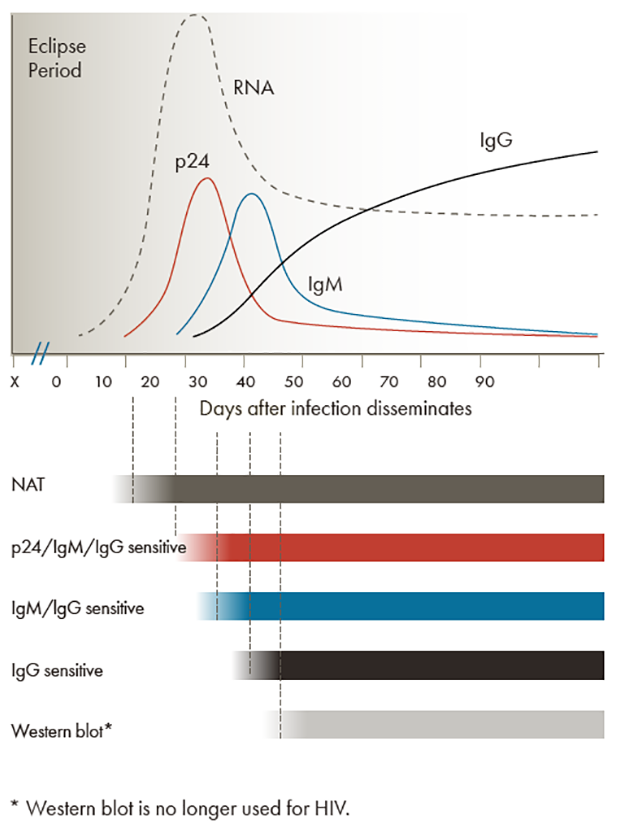
- Nucleic acid tests (NATs) — detects HIV ribonucleic acid (RNA)
- Antigen/antibody combination tests — detects HIV p24 antigen as well as HIV immunoglobulin M (IgM) and immunoglobulin G (IgG) antibodies
- Antibody tests — detects HIV IgM and/or IgG antibodies
Following an exposure that leads to HIV infection, the amount of time during which no existing diagnostic test is capable of detecting HIV is called the eclipse period.2
The time between potential HIV exposure and an accurate test result is referred to as the window period. Improvements in testing technology continue to reduce the detection window period, and, therefore, the time to diagnosis and treatment of early HIV infection. As seen in the figure, each type of HIV test has its own testing window, with the NAT capable of detecting HIV the earliest, followed by the antigen/antibody combination test, and lastly, the antibody test.
Learn more about FDA-approved Tests for HIV.
Routine Screening Should Be Implemented Using an “Opt-Out” Approach
When an Opt-Out approach is implemented, patients should be informed (e.g., through a patient brochure, practice literature/form, or discussion) that an HIV test will be included in the standard preventive screening tests, and that they may decline the test (opt-out screening).1 A patient’s decision to decline testing should be noted in their medical record. HIV prevention counseling should not be a requirement for HIV testing.
- Risk assessment should be included as part of routine primary care visits for all sexually active patients.
- Individuals at high risk may need to be screened more frequently.
- Prevention counseling also may be needed for patients at high risk for acquiring HIV but should not be required for general testing.
Why Routine, Opt-Out HIV Screening1
Conducting risk-based screening may fail to identify persons with HIV
- People <20 years of age
- Women
- Including pregnant women; HIV screening should be included in the routine panel of prenatal screening.
- Members of minority races/ethnicities
- Nonurban dwellers in low-incidence areas
- Heterosexual men and women who are unaware of their risk of HIV
Many people with HIV are not diagnosed until they have advanced HIV or AIDS
Routine, opt-out screening has proved highly effective
- Removes the stigma associated with HIV testing
- Fosters earlier diagnosis and treatment
- Reduces risk of transmission
- Is cost-effective
Justification for routine HIV screening by health care providers includes the following1
- Serious health disorder that can be detected before symptoms develop
- Detectable by reliable, inexpensive, acceptable screening tests
- People diagnosed with HIV have years of life to gain if treatment is started early, before symptoms develop
- Screening costs are reasonable in relation to anticipated benefits
HIV self-testing allows people to take an HIV test and find out their result in their own home or other private location. The availability of HIV self-tests in the US may help increase awareness of HIV infection for people who wouldn’t otherwise get an HIV test. While HIV self-tests are available for retail purchase by consumers, CDC encourages health departments to consider HIV self-testing as an additional testing strategy to reach persons most affected by HIV. Findings from self-testing research and additional resources provided below may be helpful if you are considering offering HIV self-testing in your program.
Home Specimen Collection Kit
A home specimen collection kit can be used to test for HIV and sexually transmitted infection (STI). Home collection kits can be ordered by physicians and are covered by most insurance plans. Some laboratories have validated protocols for testing home-collected samples for the panel of tests required for those initiating or continuing PrEP.
Specimen kits are mailed to the patient’s home and contain supplies to collect blood from a fingerstick or other appropriate method (e.g. self-collected swabs and urine). The kit is then mailed back to the lab with test results returned to the clinician who acts on results accordingly. This laboratory-conducted test is sensitive enough to detect recent HIV infection.
More information on home specimen collection kits for HIV and other tests required for PrEP patients will be added to this Web page as it becomes available, including additional laboratories providing this service.
Self-Testing for PrEP
CDC has developed guidance for providing PrEP when facility-based services and in-person patient-clinician contact is limited. Quarterly HIV testing should be continued for patient safety. While lab-only visits for assessment of HIV infection and other indicated tests for the provision of PrEP are preferred, when these are not available or feasible, CDC recommends considering two additional options: home specimen collection kits, which are sensitive enough to detect recent HIV infection; or self-testing via an oral swab-based test.
Although HIV self-tests are usually not recommended for PrEP patients due to their lower sensitivity in detecting recent HIV infection during PrEP use, clinicians could consider use of these tests when other options are not available.
15% of partners tested by Partner Services were positive for HIV and previously undiagnosed.
What Is Partner Services?
Partner Services provides an array of free services to people with HIV or other sexually transmitted diseases (STDs, such as syphilis, gonorrhea, and chlamydia) and their partners. Partner Services is a function of local and state health department staff, who help to identify and locate sexual or drug injection partners to inform them of their risk for HIV and to provide them with testing, counseling, and referrals for other services.
For partners who test positive, Partner Services can provide linkage to treatment and care, risk-reduction counseling, and other services.
For those who test negative, Partner Services can provide them with information on various HIV-prevention methods, including pre-exposure prophylaxis (PrEP), condoms, and other sexual and drug-use options. For partners at high risk for HIV, consider PrEP. PrEP is a powerful HIV-prevention tool and has been shown to be about 99% effective in reducing the risk of sexual HIV transmission.
Additionally, access to other services may lead to reductions in high-risk sexual and drug-use behaviors.
Partner Services Programs Reduce HIV Transmission by Helping Your Patients Inform Partners of Their HIV Status
Health Care Provider Role in Initiating Partner Services
While you are not expected to take on the role of partner notification yourself, it is very helpful for you to educate your patients about Partner Services and its importance in preventing HIV transmission.
For Patients Being Tested for HIV/STDs
- Talk with your patients about Partner Services and let them know that if they test positive for a reportable disease, they may be contacted by someone from the health department.
- Discuss how Partner Services can help your patients and their sexual or drug injection partners through early access to testing, treatment, and other services.
- Emphasize the importance of participating in the Partner Services process as a way to help stop the transmission of HIV/STDs.
- Conduct brief discussions with your patients on how to reduce high-risk sexual and drug-use behaviors.
Discussing Sexual Health With Your Patients
Tips for Asking Sensitive Questions
Transition to asking sensitive questions. Let your patient know that you ask these questions of everyone. If a partner, relative, or caregiver is in the room, ask that person to step into the waiting room. He or she can be invited back after the examination.
“ I’m going to ask you a few questions about your sexual health. Since sexual health is very important to overall health, I ask all my patients these questions.
Before I begin, do you have any questions or sexual concerns you’d like to discuss? ”
Screening In Clinical Settings
- CDC recommends that individuals between the ages of 13 and 64 get tested for HIV at least once as part of routine health care and those with risk factors get tested more frequently. A general rule for those with risk factors is to get tested at least annually.
- CDC recently released specific guidance for HIV screening for gay, bisexual and other men who have sex with men (MSM). CDC recommends that clinicians screen asymptomatic sexually active MSM at least annually. Furthermore, clinicians should consider the benefits of more frequent screening (e.g. once every 3 or 6 months) for individual MSM at increased risk for HIV Infection.
How soon can clinicians rule out infection?
CDC recently published research findingsexternal icon that estimate the window period for 20 U.S. Food and Drug Administration (FDA)-approved HIV tests. The study showed that laboratory testing using antigen/antibody tests detects HIV infection sooner than other available tests that detect only antibodies. If a person gets a laboratory-based antigen/antibody test on blood plasma less than 45 days after a possible HIV exposure and the result is negative, follow-up testing can begin 45 days after the possible HIV exposure. For all other tests, CDC recommends testing again at least 90 days after exposure to be sure that a negative test result is accurate.
When should clinicians start treatment for HIV?
Data from a National Institutes of Health sponsored trialexternal icon indicates there is a clear personal advantage to diagnosis soon after HIV infection and starting therapy early in the course of infection. The study further highlights the importance of routine HIV testing and the potential impact of early treatment on better health outcomes.