Here is the link to the show notes and podcast of Podcast 98 – Cyclic (Tricyclic) Antidepressant Overdose; May 14, 2013 by Dr. Scott Weingart.
[Note to myself: Whenever I review this post, I also need to review “CritCases 1: Massive TCA (Tricyclic Antidepressant Overdose)” – Help From Emergency Medicine Cases
Posted on March 17, 2019 by Tom Wade MD.]
I have included the show notes of Podcast 98 in this post. The posts in this blog are my study notes [peripheral brain] and going through show notes this way helps to fix them in my mind.
Podcast 98 – Cyclic (Tricyclic) Antidepressant Overdose by 37 Comments
Dr. Weingart begins:
This was a 28 year old male found by his room-mates and he was unconscious. When EMS got there he was seizing. And because the patient was too awake they couldn’t intubate. They gave two milligrams of Ativan which didn’t terminate the seizure initially. Right has they pulled up to our to the doorstep of our hospital, the seizures stopped. And they brought the patient in. And the patient had vomit in the mouth and the nose. They were still bagging the patient. The patient was responsive to pain. [I] looked up at the monitor and the blood pressure was 80/40. There were no signs of trauma and didn’t quite know where to go on this.
So we do what we always do if you’re a good emergency physician, which is you take care of the A-B-Cs.
So to get a better handle on what was going on, I didn’t want to do a full RSI [Rapid Sequence Induction]. So what we did was to perform a Rapid Sequence Airway. I gave a little bit of ketamine and a little propofol. I think we gave 20 mg of ketamine and 10 mg of propofol and push dose epi*
I think we gave 20 micrograms [of epinephrine]. And we got a decent blood pressure. Got the blood pressure up to greater than 100 systolic and popped in an LMA which requires a much lesser level of anesthesia then placing a formal ET tube and gives us some time to assess the patient. And I put the patient on the ventilator with the LMA in place. This is an intubating LMA but it doesn’t matter for what we did subsequently.
*[My note: 2 cc of the 1:100,000 push dose epi (10 micrograms of epinephrine per ml) we should always have made up and immediately available in this sort of situation.]
And now we started to get a handle on things.
Start here at 1:50
Dr. Weingart diagnosed tricyclic overdose in a patient who came in seizing and responsive only to pain and he was being bagged by the EMTs. The patient was hypotensive and he had vomitus in his mouth and throat. The seizure was treated with benzodiazepine and stopped. He was suctioned and because he was hypotensive, Dr. Weingart elected not to do an RSI but rather do an Rapid Sequence
I had a crazy case of Tricyclic Overdose while on an overnight shift at Janus General.
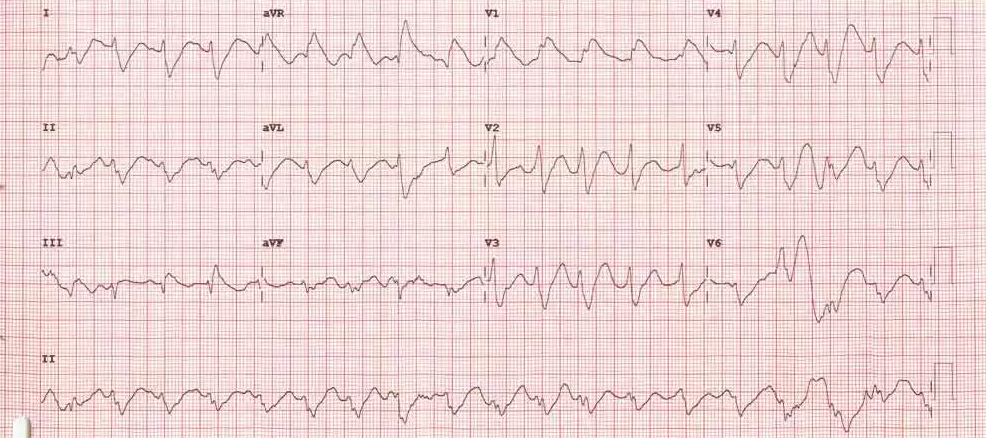
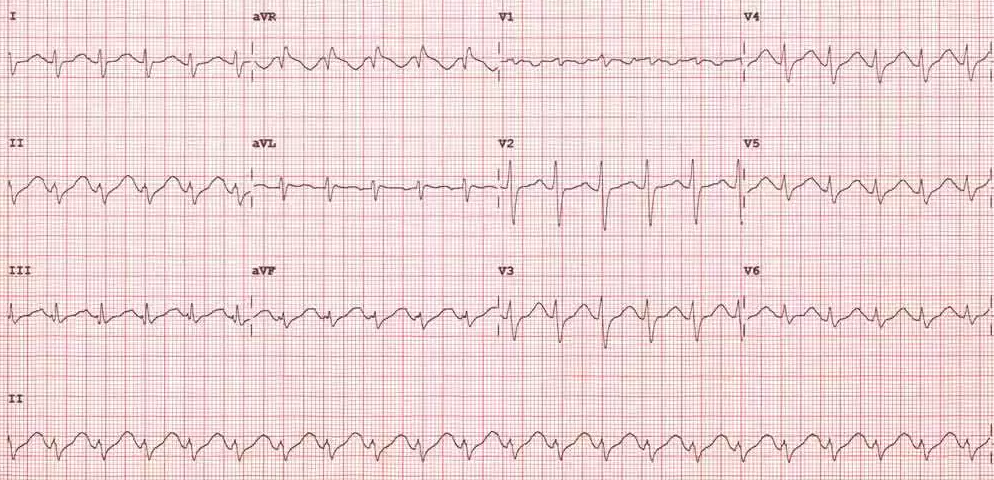
Initial and Post-Treatment EKGs
Initial
Post Treatment
List of Tricyclic Agents from Wikipedia.org
- Amitriptyline (Tryptomer, Elavil)
- Amitriptylinoxide (Amioxid, Ambivalon, Equilibrin)
- Butriptyline (Evadyne)
- Clomipramine (Anafranil)
- Demexiptiline (Deparon, Tinoran)
- Desipramine (Norpramin, Pertofrane)
- Dibenzepin (Noveril, Victoril)
- Dimetacrine (Istonil, Istonyl, Miroistonil)
- Dosulepin/Dothiepin (Prothiaden)
- Doxepin (Adapin, Sinequan)
- Imipramine (Tofranil, Janimine, Praminil)
- Imipraminoxide (Imiprex, Elepsin)
- Lofepramine (Lomont, Gamanil)
- Melitracen (Deanxit, Dixeran, Melixeran, Trausabun)
- Metapramine (Timaxel)
- Nitroxazepine (Sintamil)
- Nortriptyline (Pamelor, Aventyl, Norpress)
- Noxiptiline (Agedal, Elronon, Nogedal)
- Pipofezine (Azafen/Azaphen)
- Propizepine (Depressin, Vagran)
- Protriptyline (Vivactil)
- Quinupramine (Kevopril, Kinupril, Adeprim, Quinuprine)
Additionally…
- Amineptine (Survector, Maneon, Directim) Norepinephrine-dopamine reuptake inhibitor
- Iprindole (Prondol, Galatur, Tetran) 5-HT2 receptor antagonist
- Opipramol (Insidon, Pramolan, Ensidon, Oprimol) ? receptor agonist
- Tianeptine (Stablon, Coaxil, Tatinol) Selective serotonin reuptake enhancer
- Trimipramine (Surmontil) 5-HT2 receptor antagonist and moderate-potency norepinephrine reuptake inhibitor.
And of course, the non-TCA agents…
- Diphenhydramine [This is a link to a case report of diphenhydramine sodium channel toxicity
- Cocaine
- Cyclobenzaprine (I add this one to the list, b/c there can be TCA-like effects in toxicity, but it seems the potential for cardiac effects is markedly less though still possible. (J Emerg Med 1995;13(6):781-5) This one is from Bryan Hayes)
Pharmacologic Effects of TCAs
K+ Channel Blockade QTC Prolongation NE & Serotonin Reuptake Inhibition Initial hypertension quickly followed by hypotension Na+ Channel Blockade QRS Prolongation
Hypotension — depresses myocardial contractility
Ventricular dysrhythmias
Brugada-like findings on EKGMuscarinic Anticholinergic Receptor Antagonism Anticholinergic Toxidrome Antihistaminergic CNS stimulation or sedation Alpha1 Adrenergic Antagonism Hypotension GABA-A Receptor Blockade Seizures This chart was taken from the excellent Resus Review Blog by Charles Bruen
Sodium Bicarbonate
Increases amount of drug in non-ionized form and may decrease binding to Na-channels [cite]11482860[/cite]
May need many, many amps. For some reason the sodium and the bicarb don’t rise significantly in severe toxicity
My goals are QRS duration <100, hemodynamically stable, Na ~150, pH ~7.5
Electrolyte Abnormalities
Beware of hypokalemia and hypocalcemia
Send VBG with lytes at least Q1 hour
Hyperventilation
To promote alkalosis
Hypertonic Saline
If the patient is too alkalotic or out of amps of Bicarb
Sodium Acetate
Can substitute for NaBicarb. This article gives dosing recommendations and precautions.*
* Sodium acetate as a replacement for sodium bicarbonate in medical toxicology: a review [PubMed Abstract] [PMC Full Text] [Full Text PDF].
Magnesium
May help, though risk of Torsades is low as long as the patient remains tachycardic
Lidocaine
Even though lidocaine is another Na-Channel Blocker, it actually antagonizes the effects of the TCA-like mediciations. As a Vaughan Williams Class IB agent, For additional information, this review discusses the pertinent issues.[cite]https://www.ncbi.nlm.nih.gov/pubmed/20507243[/cite]
VasoPressors
Norepi or Epi
Intralipids
Certainly for cardiac arrest and probably for hypotension/increasing pressor necessity
For this or any other Lipid Question, you need to go immediately to the Lipid Rescue Site
You can find the Lipid Administration Instruction Sheet there, which should be hanging somewhere on the wall of your ED.
ECMO
The last resort for tox instability
Want More?
My friends Sean Nordt and Stu Swadron did a great EM:RAP episode on this 2 months ago
Here is a review and guideline article.