This post has resources on:
- Emergency management of pulmonary hypertension
- Primary care diagnosis of pulmonary hypertension
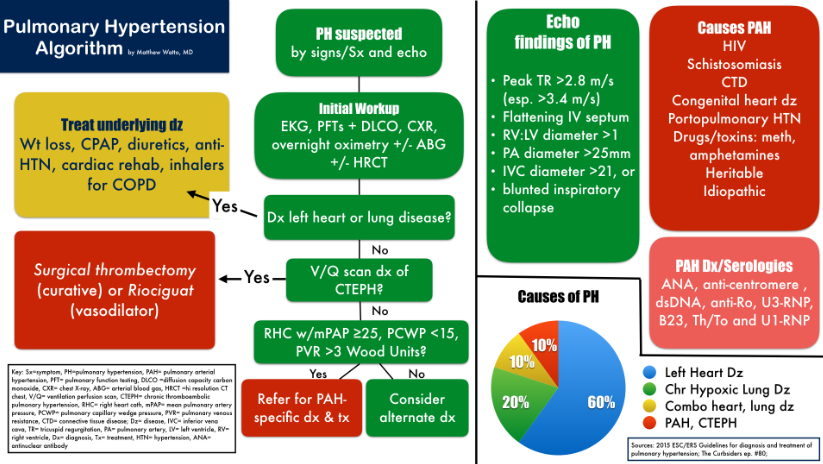
- Unexplained dyspnea on exertion should lead to consideration of the evaluation below in the chart from the Curbsiders.
- Echocardiographic assessment of pulmonary hypertension
Here is the abstract from Pulmonary Hypertension and Right Ventricular Failure in Emergency Medicine, 2015 that explains why it is so important for all clinicians to be alert to the possibility of pulmonary hypertension:
Pulmonary hypertension is a hemodynamic condition, defined as a mean pulmonary artery pressure by right-sided heart catheterization of at least 25 mm Hg at rest. It is classified into 5 general groups based on the underlying cause, with left ventricular failure and chronic obstructive pulmonary disease being 2 of the most common causes in the United States. Although the specifics of the pathophysiology will vary with the cause, appreciating the risks of pulmonary hypertension and right ventricular failure is critical to appropriately evaluating and resuscitating pulmonary hypertension patients in the emergency department (ED). Patients may present to the ED with complaints related to pulmonary hypertension or unrelated ones, but this condition will affect all aspects of care. Exertional dyspnea is the most common symptom attributable to pulmonary hypertension, but the latter should be considered in any ED patient with unexplained dyspnea on exertion, syncope, or signs of right ventricular dysfunction. Patients with right ventricular failure are often volume overloaded, and careful volume management is imperative, especially in the setting of hypotension. Vasopressors and inotropes, rather than fluid boluses, are often required in shock to augment cardiac output and reduce the risk of exacerbating right ventricular ischemia. Intubation should be avoided if possible, although hypoxemia and hypercapnia may also worsen right-sided heart
function. Emergency physicians should appreciate the role of pulmonary vasodilators in the treatment of pulmonary arterial hypertension and recognize that patients receiving these medications may rapidly develop right ventricular failure and even
death without these therapies. Patients may require interventions not readily available in the ED, such as a pulmonary artery
catheter, inhaled pulmonary vasodilators, and mechanical support with a right ventricular assist device or extracorporeal membrane oxygenation. Therefore, early consultation with a pulmonary hypertension specialist and transfer to a tertiary care center with invasive monitoring and mechanical support capabilities is advised. [Ann Emerg Med. 2015;-:1-10.]
The following chart is from #80: Pulmonary Hypertension, freeways, and cows in heart failure JANUARY 29, 2018 By MATTHEW WATTO, MD:
And here is the link to the YouTube Pulmonary Hypertension Echocardiography Protocol [37 videos]:
Embedded clips from the National Pulmonary Hypertension Service of UK and Ireland Echocardiography Protocol supported by the British Society of Echocardiography
Go to www.ph-echocardiography-protocol.com for full interactive downloadable PDF [to enlarge the text, you need to decrease the display to 33% on my display]: Echocardiographic Assessment of Pulmonary Hypertension: Standard Operating Procedure.