Note to myself and my readers: I only post excerpts from articles because doing so helps me remember the important points [spaced repetition]. Readers should download the complete article [links below] and review that.
In this post I link to and excerpt from 3.3 Pharmacological management from 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes: The Task Force for the diagnosis and management of chronic coronary syndromes of the European Society of Cardiology (ESC) [PubMed Abstract] [Full Text HTML] [Full Text PDF]. European Heart Journal, Volume 41, Issue 3, 14 January 2020, Pages 407–477.
Here are the links to the above guidelines:
Article Contents
All that follows is from 3.3 Pharmacological management.
3.3 Pharmacological management
The aims of pharmacological management of CCS patients are to reduce angina symptoms and exercise-induced ischaemia, and to prevent cardiovascular events.
Immediate relief of anginal symptoms, or the prevention of symptoms under circumstances likely to elicit angina, is usually obtained with rapidly acting formulations of nitroglycerin. Anti-ischaemic drugs—but also lifestyle changes, regular exercise training, patient education, and revascularization—all play a role in minimizing or eradicating symptoms over the long-term (long-term prevention).
Prevention of cardiovascular events targets MI and death associated with CAD, and focuses primarily on reducing the incidence of acute thrombotic events and the development of ventricular dysfunction. Strategies include pharmacological and lifestyle interventions, as detailed in the 2016 European Guidelines on CVD prevention in clinical practice.*15
*2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) [PubMed Abstract]. Eur Heart J. 2016 Aug 1;37(29):2315-2381. doi: 10.1093/eurheartj/ehw106. Epub 2016 May 23.
3.3.1 Anti-ischaemic drugs
3.3.1.1 General strategy
Optimal treatment can be defined as the treatment that satisfactorily controls symptoms and prevents cardiac events associated with CCS, with maximal patient adherence and minimal adverse events.188–191 However, there is no universal definition of an optimal treatment in patients with CCS, and drug therapies must be adapted to each patient’s characteristics and preferences.192 Initial drug therapy usually consists of one or two antianginal drugs, as necessary, plus drugs for secondary prevention of CVD.193 The initial choice of antianginal drug(s) depends on the expected tolerance related to the individual patient’s profile and comorbidities, potential drug interactions with co-administered therapies, the patient’s preferences after being informed of potential adverse effects, and drug availability. Whether combination therapy with two antianginal drugs [e.g. a beta-blocker and a calcium channel blocker (CCB)] is superior to monotherapy with any class of antianginal drug in reducing clinical events remains unclear.194–197
Beta-adrenergic blockers or CCBs are recommended as the first choice, although no RCT to date has compared this strategy to an alternative strategy using initial prescription of other anti-ischaemic drugs, or the combination of a beta-blocker and a CCB.191,195 The results of a network meta-analysis of 46 studies and 71 treatment comparisons supported the initial combination of a beta-blocker and a CCB.198 The same meta-analysis suggested that several second-line add-on anti-ischaemic drugs (long-acting nitrates, ranolazine, trimetazidine, and, to a lesser extent, ivabradine) may prove beneficial in combination with a beta-blocker or a CCB as first-line therapy, while no data were available for nicorandil. However, it should be noted that the study pooled RCTs using endpoints of nitrate use, angina frequency, time to angina or to ST-segment depression, and total exercise time, and no study or meta-analysis has yet assessed with sufficient power the influence of combining a beta-blocker or a CCB with a second-line anti-ischaemic drug on morbidity or mortality events.198 Regardless of the initial strategy, response to initial antianginal therapy should be reassessed after 2–4 weeks of treatment initiation.
3.3.1.2 Available drugs
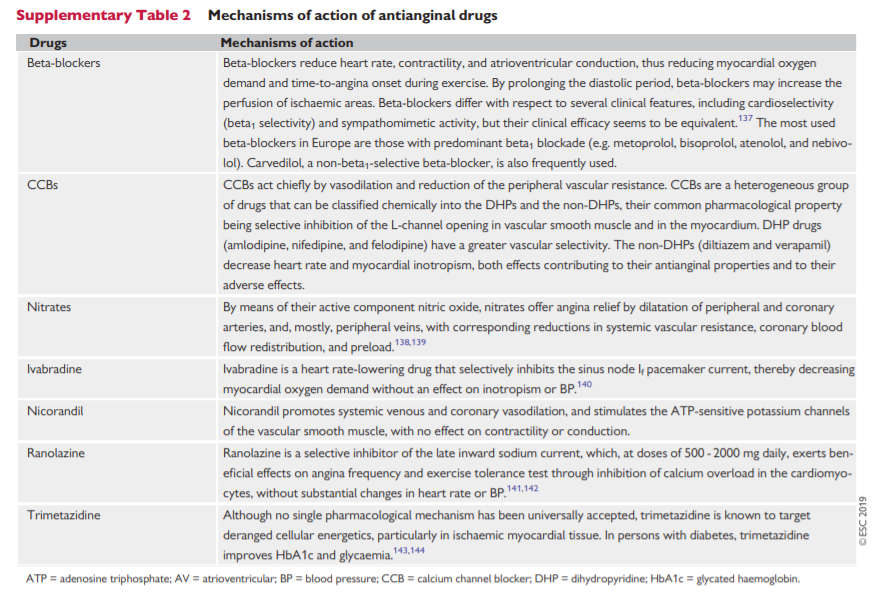
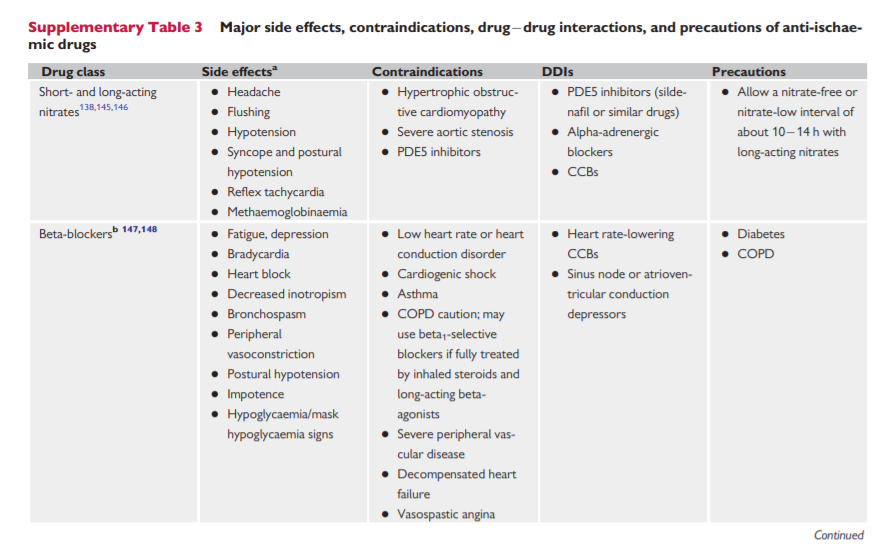
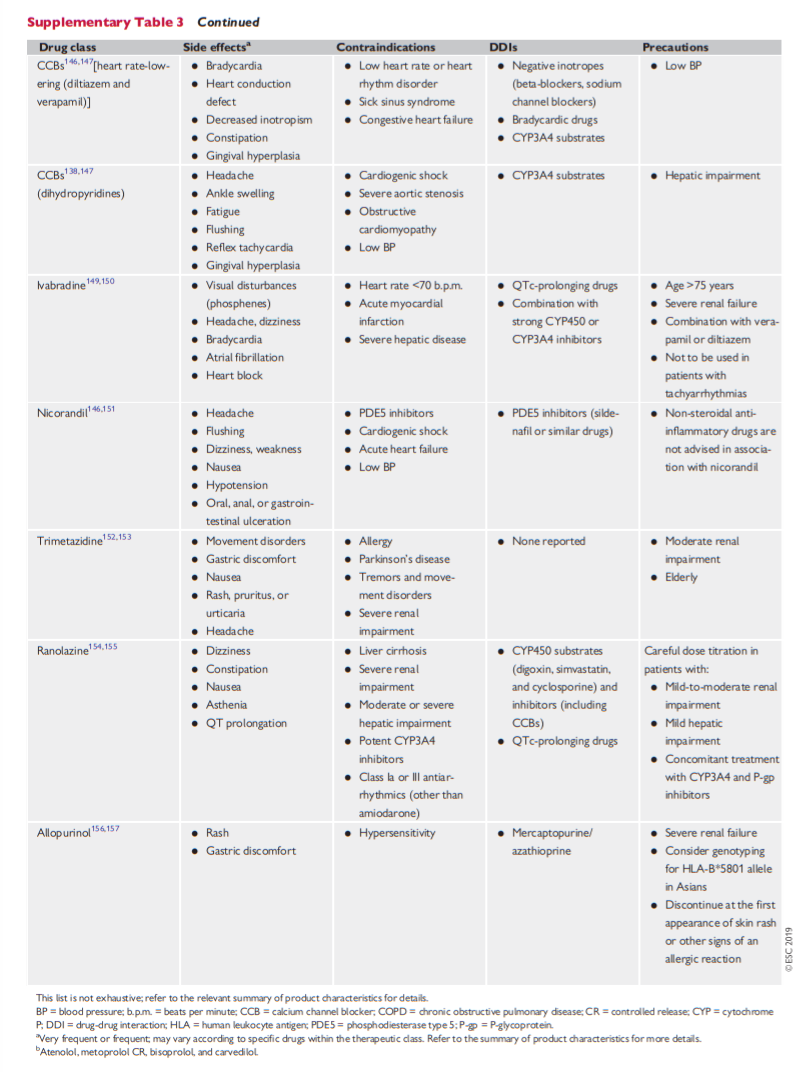
Anti-ischaemic drugs have proved benefits regarding symptoms associated with myocardial ischaemia but do not prevent cardiovascular events in most patients with CCS. Supplementary Table 3 in the Supplementary Data summarizes the principal major side effects, contraindications, drug–drug interactions, and precautions relating to anti-ischaemic drugs. Supplementary Table 2 summarizes the main mechanisms of action of anti-ischaemic drugs.
Nitrates
Short-acting nitrates for acute effort angina