This blog contains the medical topics that I have reviewed. It is my peripheral brain. The WordPress search built into the software makes it easy to keep track of the topics I have reviewed.
So in this post, I’m trying something new. I typed “intussusception” into the blog’s search box. And I’m listing post that comes up. And I’ll see how long a quick review of each of the posts takes and see if it helps in my general review.
So, when I typed “intussusception” into the search box, 28 posts came up. So here’s the list. And there are excerpts from many (but not all) of the posts. I’ll see if this is a good way to review.
Links To And Excerpts From An Approach To Intussusception From PedsCases With An Additional Recommendation
My additional recommendation: In every pediatric patient of any age with abdominal symptoms (pain, decreased appetite, abnormal vital signs, nausea, vomiting, or diarrhea), our job is to always look for and rule out dehydration, sepsis, surgical abdomen*, and serious metabolic … Continue reading
Idiopathic intussusception occurs primarily in infants from 3 months to 3 years old, peaking between 5-9 months. Risk factors for intussusception include: male sex and co-existing/recent viral illnesses (adenovirus, rotavirus and HHV 6).
Imaging is key for the diagnosis of intussusception. Ultrasound is the preferred modality due to its superior safety profile and higher sensitivity and specificity for the diagnoses of intussusception.
In the emergency setting, supine, frontal and left lateral decubitus abdominal radiographs are often used to rule
out other potential conditions such as the presence of free peritoneal air. These radiographs can occasionally detect intussusception but cannot rule it out.
“Pediatric Emergency Ultrasound: Deep Dive on POCUS for Intussusception” – Help From ACEP With Additional Resources
Pediatric Emergency Ultrasound: Deep Dive on POCUS for Intussusception By Lilly A. Bellman, MD (@LillyBellman) & Manpreet Singh, MD (@MPrizzleER) What follows are excerpts from the above: Case Your nurse is about to fill three rooms with vomiting children – … Continue reading
Case
Your nurse is about to fill three rooms with vomiting children – must be another AGE virus going around! Two of the kids have classic vomiting with diarrhea and had a sick contact, and look very well. They’ll be easy Zo-Po-Go (ie Zofran, PO challenge, Go Home)!
The third one, however, is a 2-year-old now on his second day of vomiting (non-bilious, non-bloody), has no diarrhea, no fever, and the parent tells you they’ve been very “irritable.” It’s hard to examine his belly as he starts crying the minute you get close (even with all your great pediatric flair). His vitals are “OK” – somewhat tachycardic but probably was crying, normal BP, RR, SpO2, and temperature.
So you’re thinking differential: Could still be AGE? However, you’re also worried about other pathologies, such as appendicitis, intussusception, or testicular torsion (though normal GU exam).
And also don’t forget to consider other causes of just vomiting without accompanying diarrhea such as diabetic ketoacidosis, increased intracranial pressure, or other causes of bowel obstruction.
Reviewing Acute Abdominal Pain From PedsCases
Today, I reviewed and link to PedsCases‘ Acute Abdominal Pain, by Peter.MacPherson Jun 22, 2010: This episode covers an approach to children with acute abdominal pain. The podcast covers an approach to history, an approach to physical examination, discusses investigations and … Continue reading
Dr. Lewis: The first thing to consider is whether the child looks sick. If they look seriously ill, they most likely are.*
As always, vitals are important. Is the child febrile? Look for signs of hypovolemia and assess their fluid status.*
[*The above is the most important part of the pediatric evaluation. A patient who looks sick is potentially critically ill and needs to be transferred from the office or urgent care to the emergency department. ]
[Text in brackets is not from the PedsCases script. Rather it is my thoughts on the material. It’s purpose is to remind me of the implications of the podcast.]
[*In the emergency department, the patient should receive close monitoring of his/her vital signs [BP, cardiac monitoring, RR, T, oximetry, and capnography]. Any abnormalities in the patient’s physical exam should be addressed immediately.]
[*And in these cases of acute abdominal pain, an immediate pediatric surgery consult should be strongly considered.]
Links To And Excerpts From An Approach to Pediatric Bowel Obstruction From PedsCases
In this post, I review, link to, and excerpt from PedsCases An Approach to Pediatric Bowel Obstruction, by Kevin.Verhoeff Jun 19, 2020: This podcast presents an approach to diagnosing and managing an important pediatric emergency, pediatric bowel obstruction. Compared to … Continue reading
Given the large differential for bowel obstruction in children it is helpful to break it up into conditions that present in the newborn period, and other conditions that present later in infancy and childhood.
A 2-week-old girl is brought to the emergency room with acute onset bilious vomiting. Further history demonstrates that she passed meconium in the first 24 hours, was doing well with 2
normal yellow stools every day with no blood or melena, but on presentation today has not stooled in the last 24 hours. She has been febrile and is irritable with distention and peritoneal findings on exam.In a second case, you are on your pediatrics rotation and rounding on a newborn boy with known Down syndrome. The boy’s vitals are within normal ranges but after speaking with the parents they are concerned because he has been vomiting bilious material since delivery shortly after every feed. He has also not had any bowel movements. On exam, the boy appears well, but has not tolerated any oral intake since birth.
Neonatal causes for bowel obstruction occur primarily due to congenital processes. The most common embryological defect is malrotation.
The first case represents malrotation and volvulus,and is one of the pediatric presentations that may have “RED FLAG” symptoms requiring immediate attention. Any patient presenting with new onset BILIOUS emesis, marked abdominal distension, associated with a fever, elevated white blood cell count, and physical signs of localized and/or generalized peritoneal findings should be considered a surgical emergency. These findings signify an acute abdomen. A stable patient with these symptoms may be investigated with an urgent upper GI contrast study to exclude malrotation with volvulus, even in the middle of the night. An unstable patient such as the one in our case may better served with an urgent laparotomy.
Other congenital issues and causes for neonatal bowel obstruction exist as well.
Your differential for neonates should also include meconium ileus (which is often the first clinical sign of cystic fibrosis), Hirschsprung disease, abdominal wall defects (including gastroschisis and omphalocele), and imperforate anus. Finally, incarcerated inguinal hernia is a common and often overlooked cause of bowel obstruction in the premature population. To learn more, there are great PedsCases podcasts on both Hirschsprung Disease and Pediatric Hernias.
Infancy and Childhood Differential Diagnoses:
After approximately the first 4-weeks of life up to 2 years of age your differential should shift to consider other causes of bowel obstruction. Consider the following 2 clinical cases:
You are seeing a 6-week-old first born male in a pediatrician’s clinic who appears unwell. His father tells you that for the last 2 weeks he has had more frequent episodes of non-bilious, projectile emesis that occurs after being breast fed. The dad tells you that recently, he has projectile vomiting after each feed, that he is lethargic, has been having fewer stools with no
bowel movements in the last 2 days, appears to be losing weight, and has fewer wet diapers.
On exam, you recognize a 6-week old child with sunken eyes and delayed capillary refill. Abdominal exam is benign with no distention, no pain, and a scaphoid abdomen.In the second case, a 15-year-old male with a history of neurodevelopmental delays, G-tube feeds and a fundoplication presents with abdominal pain, bilious vomiting, and obstipation. He is not tolerating any feeds without vomiting. On exam, you note surgical scars on the abdomen, with significant distention, and tenderness to light percussion.
The differential diagnosis during infancy and childhood should include things such as intussusception, pyloric stenosis, annular pancreas, necrotizing enterocolitis associated adhesions, surgical adhesions, neoplasm, and cystic fibrosis. Of course, don’t overlook the possibility of functional constipation in these patients. To learn more, there are great PedsCases podcasts on intussusception, and necrotizing enterocolitis.
Of note, another diagnosis that should always be part of any differential diagnosis for acute abdominal symptoms is appendicitis. Appendicitis is known to be a great mimicker of multiple pathologies. A perforated appendix and abscess can cause a non-mechanical bowel obstruction. Young children may present with a several days’ history of vague abdominal
symptoms, fever, obstruction and emesis.In the first case we discussed, the infant has had progressive worsening of symptoms, nonbilious but projectile vomiting after feeds, and appears quite unwell. There is no mention of
abdominal distention, pain, or peritoneal signs and the progressive nature and other signs would suggest pyloric stenosis as the diagnosis. Symptoms were not immediate at birth,and worsened as the pylorus became tighter as it hypertrophied. The vomit in pyloric stenosis is not bilious
because the obstruction is in the pylorus of the stomach, proximal to where bile is released into the GI tract. In these cases, you may also note an “olive pit” like mass in the patient’s
epigastrium and commonly find hypochloremic, hypokalemic, metabolic alkalosis on the bloodwork. Abdominal ultrasound is the gold standard imaging modality and can demonstrate a
ultrasound is non-diagnostic and would show lack of contrast flow past the stomach.In the second case, a complex male with a history of abdominal surgery presented with classic signs of a bowel obstruction due to adhesions. This is important to consider in any patient with a
history of prior abdominal surgery. An abdominal X-ray showed dilated loops of bowel with multiple air-fluid levels, supporting the diagnosis.
Links To And Excerpts From “Information for Pediatric Healthcare Providers” On COVID-19 From The CDC
In this post I link to and excerpt from the CDC‘s Information for Pediatric Healthcare Providers updated Aug 19, 2020. Here are excerpts from the above: On This Page Infections Among Children Symptoms and Severity Testing and Isolation Laboratory and … Continue reading
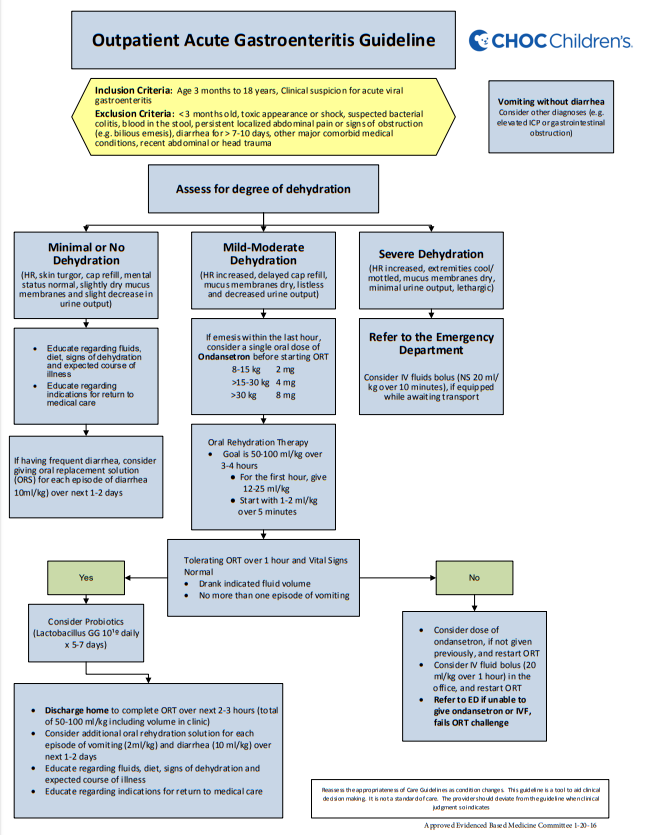
The Outpatient [Pediatric] Acute Gastroenteritis Guideline From CHOC Children’s
Here is a copy of the flow chart of CHOC Children’s 8 page PDF on their Outpatient Acute Gastroenteritis Guideline [Link is to flow chart and PDF]: Here is the rest of the CHOC Children’s 8 page PDF: Outpatient AGE … Continue reading
Here is a copy of the flow chart of CHOC Children’s 8 page PDF on their Outpatient Acute Gastroenteritis Guideline [Link is to flow chart and PDF]:
It is important to review the rest of CHOC Children’s 8 page PDF: The Outpatient [Pediatric] Acute Gastroenteritis Guideline From CHOC Children’s. Link is to the CHOC guideline which has everything you need to review.
Links To PedsCases’ “Approach to Abdominal Mass Part 1 With Additional Resources
Here is a list of all the types of resources available on PedsCases, Categories. In this post I link to and excerpt from PedsCases’ Approach to Abdominal Mass Part 1 by Kieran.Purich Oct 15, 2017 [Link to the podcast] [Link to … Continue reading
The above is a useful resource but if appropriate, just review the entire post.
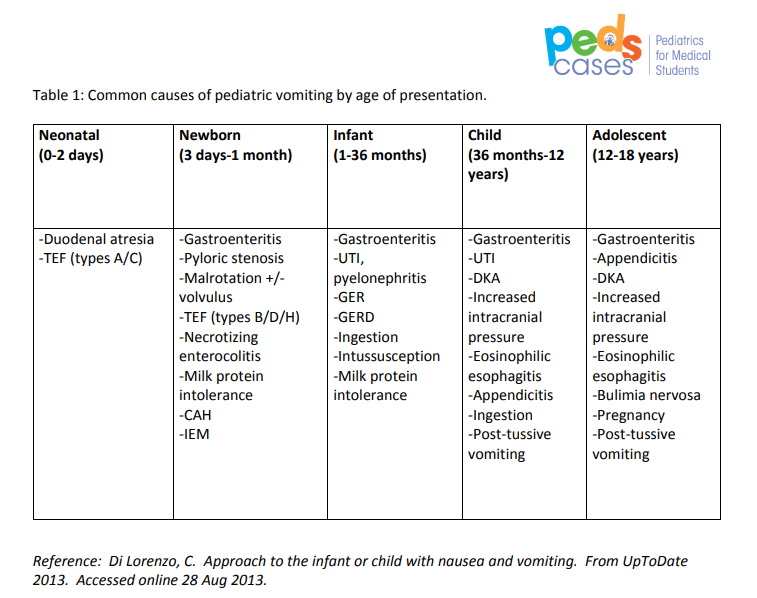
Links To PedsCases Approach to Pediatric Vomitting Part 1
Here is a list of all the types of resources available on PedsCases, Categories. Today I reviewed PedsCases Approach to Pediatric Vomitting Part 1. I’ll be reviewing Pediatric Vomitting Part 2 in an upcoming post. Here are the direct links: Approach … Continue reading
Links To PedsCases Approach to Pediatric Vomitting Part 2 With Additional Resources
Today I review PedsCases Approach to Pediatric Vomiting Part 2. I’ve reviewed Approach to Pediatric Vomiting Part 1 previously… Continue reading–>
The above resource is an excellent memory aid to be sure that you consider all the causes of pediatric vomiting.
Second Review Of PedsCases Pediatric GI Resources
Here is a list of all the types of resources available on PedsCases, Categories. In this post I listed PedsCases podcasts and show notes that I have reviewed over today (I plan to review each resource again individually and post … Continue reading
- Constipation
Published: Dec 27, 2018
- Inflammatory Bowel Disease
Published: Jun 27, 2019
- An Approach to Intussusception
Published: Oct 18, 2016
Pediatric Gastroesophageal Reflux by Viane Faily Dec 16, 2019 From PedsCases
In this post I link to and excerpt from the transcript of Gastroesophageal Reflux [Link is to the podcast] by Viane Faily, Dec 16, 2019. From PedsCases: This podcast will discuss the definition, pathophysiology, clinical manifestations, and management of gastroesophageal … Continue reading
Pediatric Pain Or Vomitting – A Reminder From Dr. Fox And Additional Resources
The posts on this blog are simply my medical study notes, my peripheral brain. So I after I reviewed Dr. Fox’s excellent post on Sigmoid Volvulus, I reviewed two of my previous posts on pediatric abdominal pain: Pediatric Abdominal Emergencies … Continue reading
Exploring The PedsCases Website And Its Resources
PedsCases “Pediatrics For Medical Students” [Link to Home Page] is a great podcast series. And here are other links from the site: Podcasts is the link to a 20 page list of podcasts going back to 2009. There are approximately … Continue reading
Evaluation Of Excessive Crying In The Infant and Toddler – Four Resources
Resource: (1) The role of abdominal ultrasound in the management of excessive crying in infants [PubMed Abstract] [Full Text] [Full Text PDF]. Pan Afr Med J. 2018 May 28;30:68. doi: 10.11604/pamj.2018.30.68.12058. eCollection 2018. (2) An Unusual Cause of Persistent Crying in a … Continue reading
Pediatric Abdominal Emergencies Lecture From CHOP With Additional Resources
Here is the link to The Clinical Pathways Library [a comprehensive list of the clinical pathways at the Children’s Hospital of Philadelphia (CHOP)]. For a complete list of the outstanding pediatric FOAM courses from the Children’s Hospital of Philadelphia, please see CHOP Open-access … Continue reading
A New Danger “Loperamide Abuse and Overuse” – Help From Dr. Fox Of Pediatric EM Morsels
This is a link to Dr. Sean Fox’s outstanding and important post Loperamide Abuse and Overuse published August 3, 2018 on his blog Pediatric EM Morsels. Loperamide abuse has many presentations including altered mental status. Also be sure and review my … Continue reading
“Hemolytic Uremic Syndrome (HUS): Pearls and Pitfalls” – Help From EMDocs
Hemolytic Uremic Syndrome (HUS): Pearls and Pitfalls Jan 8, 2016 from EMDocs is an excellent post. And as a bonus you can get CME for the post from FOAMbase. You can find a complete Table of Contents of all the topics covered on … Continue reading
Evaluation and Management of Pediatric Bloody Diarrhea – Help From The BMJ
These two charts from the article below are heart of the matter as far as the evaluation of pediatric bloody diarrhea: What follows are some excerpts from Management of bloody diarrhoea in children in primary care from the British Medical Journal: … Continue reading
Henoch Schonlein Purpura – Some Pearls, Resources, And A Guideline From RCHM
The features of Henoch Schonlein Purpura, the most common vasculitis affecting children can be recalled by the ARENA mnemonic [A = abdominal pain (65% of cases), R = rash (100%), E = edema, N = nephritis (40%), A = arthritis … Continue reading
Pediatric Pelvic Inflammatory Disease – Help From Dr. Fox of Pediatric EM Morsels
Dr. Fox’s post on Pediatric Pelvic Inflammatory Disease from Pediatric Emergency Medicine Morsels is outstanding. All of his posts are brief and totally relevant. What follows below is just the introduction from the post. Go and read the post. Here is … Continue reading
Henoch Schonlein Purpura – Help From Pediatric EM Morsels
The features of Henoch Schonlein Purpura, the most common vasculitis affecting children can be recalled by the ARENA mnemonic [A = abdominal pain (65% of cases), R = rash (100%), E = edema, N = nephritis (40%), A = arthritis … Continue reading
Ultrasound In The Dx of Intussception and In The Dx of Inflammatory Bowel Disease But Not For Volvulus
I found the article, Diagnostics in Inflammatory Bowel Disease: Ultrasound [links in Resources], in Google search. I was reviewing some of the cases in Case Studies In Pediatric and Emergency and Critical Care Ultrasound 2013 (an excellent book for learning … Continue reading
Pediatric Acute Abdominal Pain
The following is from Reference (1): The following is from Reference (2): Most Common Diagnoses for Pediatric Abdominal Pain in the ED In order of prevalence 1. Gastroenteritis 2. Respiratory Tract Infection (including Otitis Media, Pharyngitis and pneumonia) 3. UTI … Continue reading
Intussception From Emergency Medicine Cases #19 Part 2
The following is from EMC Episode 19 Part 2: Pediatric Gastroenteritis, Constipation and Bowel Obstruction [link is to the show notes and podcast]: INTUSSESCEPTION Prolapse of a segment of intestine into the lumen of an immediately adjacent part, and is the most … Continue reading
The Complete (To 3-7-2016) List of Emergency Medicine Cases Podcasts
Emergency Medicine Cases is simply a treasure trove of clinical knowledge relevant to every primary care physician, nurse, nurse practioner, and physician’s assistant. The following is a list of all the Emergency Medicine Cases podcasts PDFs [the preceding link is to … Continue reading
Intussception: YouTube Videos and Emedicine Excerpts
Outstanding YouTube video by Dr. Larry Mellick, Life Threatening Intussception Emergency, showing a child with intussception and showing the reduction with an air contrast enema. Entered ultrasound for intussception into YouTube search and the following came up https://www.youtube.com/results?search_query=ultrasound+for+intussusception and found: [Ultrasound for … Continue reading
Hirschsprung Disease and Hirschprung Enterocolitis
Dr. Klauer, an emergency physician, in a recent Audio Digest Pediatrics lecture (1), discussed the case of 12-day-old infant boy who had had no bowel movements for two days. He was formula fed and he had no fever and no … Continue reading
Is Your Infant or Child’s Abdominal Pain Serious? Should You Go to the Doctor?
Abdominal pain is common in infants and children and most of the time it is not serious. The following are some questions you can ask yourself to help decide if the child needs to see a doctor. (1) How bad … Continue reading