In this post I link to the CoreIM shownotes and podcast, 5 Pearls on Proton Pump Inhibitors. Posted: August 29, 2018. By: Dr. Cary Blum, Dr. Martin Fried and Dr. Shreya P. Trivedi.Graphic: Dr. Michael Shen.Audio: Harit Shah. Peer Review: Dr. Peter Stanich.
What follows are excerpts from the outstanding shownotes:
[Questions Answered In The] 5 Pearls On Proton Pump Inhibitors
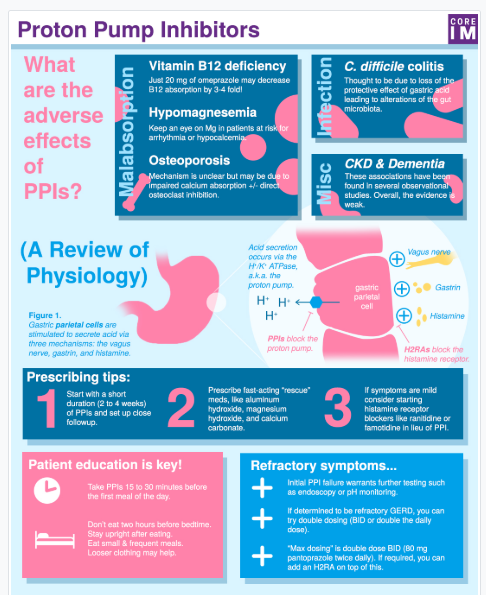
- What are associated adverse effects for patients are on long-term PPIs? (2:02)
- What are some strategies to get your patient off PPIs? (10:57)
- How do histamine-2 (H2) receptor antagonists blockers work and how can it explain why H2 blockers might not be as effective as PPIs? (13:30)
- How should you educate patients to take PPIs to get the maximize benefit? (16:48)
- How do you manage ongoing symptoms in patients on PPIs? (21:41)
Pearl 1:
What are [the] associated adverse [medical] effects for patients that are on long-term PPIs? (2:02)
S: Let’s pause [here] and talk about some of the PPI-induced medical problems that you were worried about in this patient specifically but then also other side effects we should all be familiar with.
C: Right so when I think about adverse effects of PPI I divide them into two big buckets – those related to malabsorption and those related to infection.
M: Nice I do like having a schema to organize these ideas. Cary I’ve recently heard about chronic kidney disease associated with PPIs – that doesn’t seem like either malabsorption or infection. How would you classify that?
C: Well, I should admit, there’s also likey a third “miscellaneous” category, of conditions that are associated with PPI use but the mechanism is very sketchy. CKD is in this category. Its weakly but statistically associated with PPI use in observational studies but the absolute risk comes out to only 1 to 3 additional cases in 1000 patient years.
S: I think dementia probably belongs third miscellaneous category.
C: For sure. Early studies also showed an association between PPIs and dementia, but more recent studies have failed to replicate these findings.
C: Three main complications related to malabsorption – Vitamin B12 deficiency, low magnesium levels and osteoporosis.
S: B12! I’m starting to see the connections with your patient Cary. Vitamin B12 levels are often checked in the initial workup of reversible causes of dementia.
C: That’s definitely true and the combination of initial memory complaints of my patient and long-term PPI use led me to send off levels, which were super low. I started repleting right away.
M: Alright, and did his memory get any better?
C: Well, not exactly… looks like his cognitive issues are bit more complicated and, like many patients, probably multifactorial, but I’m glad we caught that B12 deficiency before it did become a problem.
M: Oh man that would have been perfect if a little B12 fixed him right up. Let’s get into the evidence behind vitamin B12 malabsorption in the setting of PPI use.
C: There is pretty strong evidence that PPIs diminish B12 absorption, but the absolute excess risk of developing vitamin deficiency is not huge–something on the order of 3 to 4 cases per 1000 person years, translating to a relative increase of 60 to 70% over patients not on PPIs.
A well-designed RCT give a pretty convincing case for causation. Healthy volunteers underwent a modified Schilling test both before and after initiating PPI therapy. The authors showed that taking just 20 mg of omeprazole decreases B12 absorption by 3-4 fold.
S: Alright, what’s the take home here, Cary?
C: My practice now is to monitor patients’ B12 levels about annually if they are on PPIs.
M: Listeners – We are in a guideline free zone here! We’d love to hear what your practice regarding B12 monitoring and long-term PPI use.
M: [So], what’s the next stop on the malabsorption express?
C: That would be hypomagnesemia comin’ up next.
M: I personally like to shorten that to “hypo-mag” because it sounds cooler on rounds
S: Hah alright. So what’s the evidence for “hypo-mag” in PPI users?
C: The absolute risk of low magnesium individual patients is likely small, but the association is convincing and PPI’s even carry an FDA warning regarding hypomagnesemia. A meta-analysis of 9 studies confirmed that people on long term PPI therapy have an almost 50% greater relative risk for low magnesium levels than a control group. We’ll link that paper in the show notes.
S: The other big thing is–low magnesium predisposes to other electrolyte problems like hypocalcemia.*
*Hypomagnesimia Updated: Aug 23, 2018
Author: Tibor Fulop, MD, PhD, FACP, FASN;from emedicine.medscape.com:Background
Abnormalities of magnesium levels, such as hypomagnesemia, can result in disturbances in nearly every organ system and can cause potentially fatal complications (eg, ventricular arrhythmia, coronary artery vasospasm, sudden death). (See Pathophysiology.) Despite the well-recognized importance of magnesium, low and high levels have been documented in ill patients, [1] as a result of which, magnesium has occasionally been called the “forgotten cation.” [2, 3]
* Hypomagnesimia can cause hypokalemia, arrythmia, hypertension, coronary artery disease, neuromuscular manifestations, osteoporosis, nephrolithiasis, diabetes, and miscellaneous conditions [from the above article].
*