Every pediatrician (whether physician, np, or pa) needs to ask at every patient encounter: Could this patient be septic? And if the answer is yes or maybe, then he or she should begin treatment.
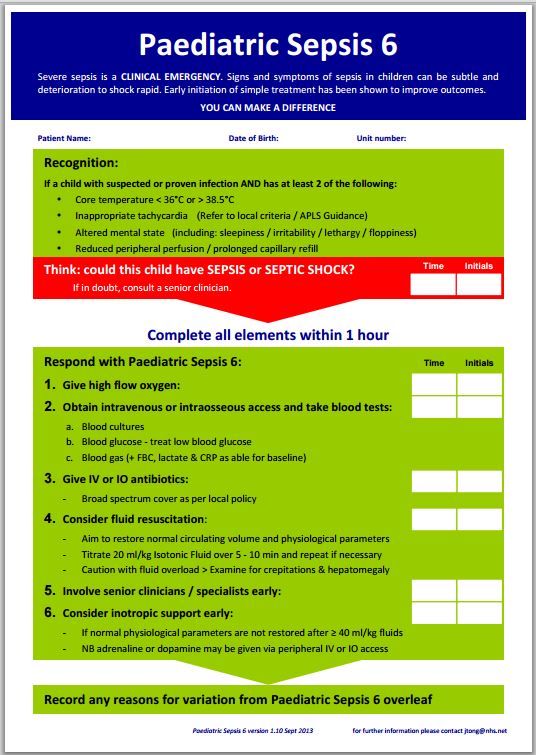
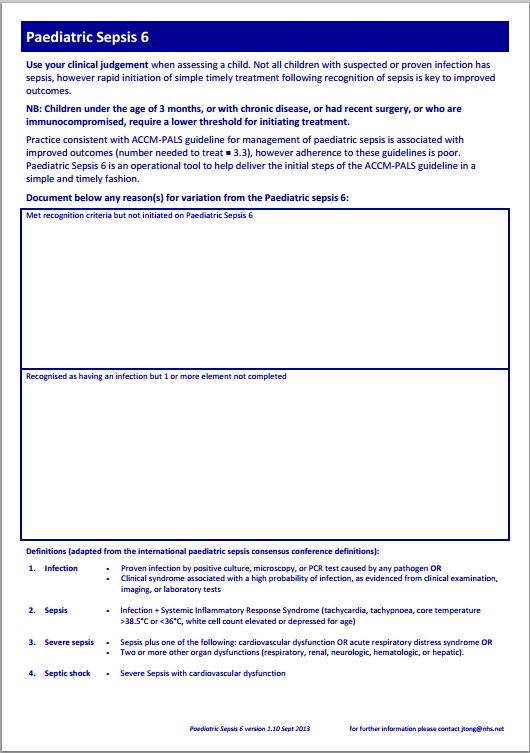
The Paediatric Sepsis 6 [2-7-2019: this link is no longer working but I’ve included a copy later in this post.]
See also the post “More Resources On the Pediatric Early Warning Score“
Posted on May 16, 2015 by Tom Wade MD. This post has direct links to outstanding Pediatric Early Warning Forms (pdfs) for each pediatric age group. And each form has age specific vital signs and suggested specific actions.
Perhaps the easiest sign to miss, especially if the heart rate was simply guestimated, would be an inappropriate tachycardia. Perhaps using an oximeter for the pulse (assuming a good pulse) or a pediatric transport monitor would be the best way to measure heart rate.
Additional Resources:
G218(P) The Paediatric Sepsis 6 Initiative [Abstract] Arch Dis Child 2014;99:A93 doi:10.1136/archdischild-2014-306237.215
More Resources On the Pediatric Early Warning Score
Posted on May 16, 2015. This post has links to everything you need to begin using the outstanding Pediatric Early Warning Score in your practice.
Pediatric Sepsis and Septic Shock
Posted on May 11, 2015 by Tom Wade MD. This post contains table of pediatric vital signs including heart rate.