Be sure and click here on Additional Resources at the end of this post for information and videos on how to prepare and use push dose pressors (push dose epinephrine).
And also here is a link to Dr. Weingart’s invaluable Stop Points podcast (which covers what to think about and do when you have a patient in septic shock on a high dose pressor drip and it’s not working).
And every patient with medical shock (non-traumatic shock) a Rapid Ultrasound in Shock and Hypotension exam. There is a reference on this crucial exam in Additional Resources (Click here. The reference has detailed information on how to perform, sequence, and interpret the RUSH exam).
These are notes that I made for myself to fix Dr. Weingart’s lecture, Vasopressor Basics EmCrit Podcast 138 in to my mind. But the podcast itself should be listened to as there is much more in the podcast than in my notes. [Link is to the show notes which also contains the link to the podcast. And as always with an EmCrit Podcast if you skip reading the listener comments and Dr. Weingart’s replies, you are missing out on a lot of great learning.]
7-25-2020 What follows are, I think, quotes from Dr. Weingart. When I posted this I must not have known how to use the quotes mark (which I do now). So I’m placing all that follows in quotes.
There are four types of shock which is inadequate tissue perfusion: Obstructive shock, hypovolemic shock, cardiogenic shock, and distributive shock.
Obstructive shock occurs when circulation is mechanically blocked: Tension pneumothorax, pericardial tamponade, pulmonary embolus.
Hypovolemic shock occurs when there is not enough blood or fluid in the pipes: Severe diarrhea, severe vomitting, external or internal bleeding.
Cardiac shock occurs when the heart is not able to pump enough blood: Primary problems intrinsic to the heart (acute myocardial infarction, myocarditis) and secondary problems (for example, the myocardial depression that can occur as a result of the inflammatory mediators of sepsis).
Distributive shock occurs when the blood vessels have dilated and their volume now exceeds the blood volume: Septic shock, neurogenic shock, anaphylaxis.
Vasopressors will only help in distributive shock because the mechanism in the three other types of shock is not vascular dilatation.
Nevertheless, if the critical perfusion pressure falls below a certain minimum in obstructive, hypovolemic, or cardiac shock, then vasopressors may be necessary as a temporizing measure.
The heart will just stop pumping effectively if the coronary perfusion pressure falls below a certain level, 65 mm MAP (mean arterial pressure).
The critical perfusion pressure for the brain is, we think, is a MAP of below 50 mm. Below this level the patient will become confused, groggy, comatose.
And with a MAP below 40 the patient will be at risk of CNS tissue damage. And will not be able to protect his airway nor be able to ventilate. So get the MAP above 40 right away however you can. If can’t get the MAP above 40 think seriously about entubating patient to protect the airway and to take as much of a load off his cardiovascular system as possible.
The coronary perfusion pressure is critical and “in general if you want a beautifully functioning heart in most people we say a MAP of 65 is necessary to allow diastolic filling of the left ventricle. And, if it gets below that point, whatever heart dysfunction you see could be as the result of something intrinsic to the heart or it could be that there is just not enough coronary perfusion pressure. “Until you fix that situation you are not going to know which one is going on. And so that is why we are always trying to keep a MAP of greater than 65 to keep the heart functioning; because the heart is what is generating flow. . . . You can’t really assess what is going on until you get that MAP of greater than 65.”
The renal perfusion pressure is also very important. And probably a MAP of 65 to 75 allows the kidneys to say, yes, we are doing okay and so we can make urine.
So the CNS perfusion pressure, coronary perfusion pressure, and renal perfusion pressure are the important parameters. And in distributive shock, vasopressors will play (along with fluid) an important role.
Sometimes, you will echo a heart with a MAP of less than 65 and it will be contracting very vigorously. But you know you need to get the MAP to 65 and so you appropriately begin a vasopressor and the MAP goes up to 65.
But then sometimes when you re-echo the heart you see that it is contracting very poorly. You did not mess up. The heart’s coronary perfusion pressure needs to be 65 and so it needs a vasopressor.The reason it is performing poorly is because before it was pumping against no resistance. Now it is having to work a lot against the resistance. You still did the right thing by getting the MAP to 65. Now you have to address increasing the cardiac output which Dr. Weingart addresses later in the lecture.
So with our vasopressor we are trying to accomplish three goals:
First, maintain an adequate perfusion pressure;
Second, to increase venous return (which is the first effect of norepinephrine, a balanced arterial and venous pressor and our vasopressor of choice) and thus you are increasing cardiac output [and hence blood pressure] by increasing preload rather than by increasing after load.
“So, instead of having to pour in 9 liters of fluid in a septic shock patient to get a certain cardiac output, a certain stroke volume, you may be able to accomplish the same goal by giving 3 liters of fluid and a touch of norepinephrine “without in any way diminishing flow. You are actually augmenting flow” and your not giving the patient too much fluid. “Every septic shock patient probably needs a little norepinephrine.”
Third, “Our last goal is to avoid gut ischemia.” If you give too much vasopressor, say, for example, because you haven’t given enough fluid, you can cause gut damage by gut ischemia. And gut ischemia can cause bacterial translocation and it may be the mechanism of serious infections post cardiac arrest or in cases of non-bacterial sepsis. For pretty much everyone our goal is a MAP 65.
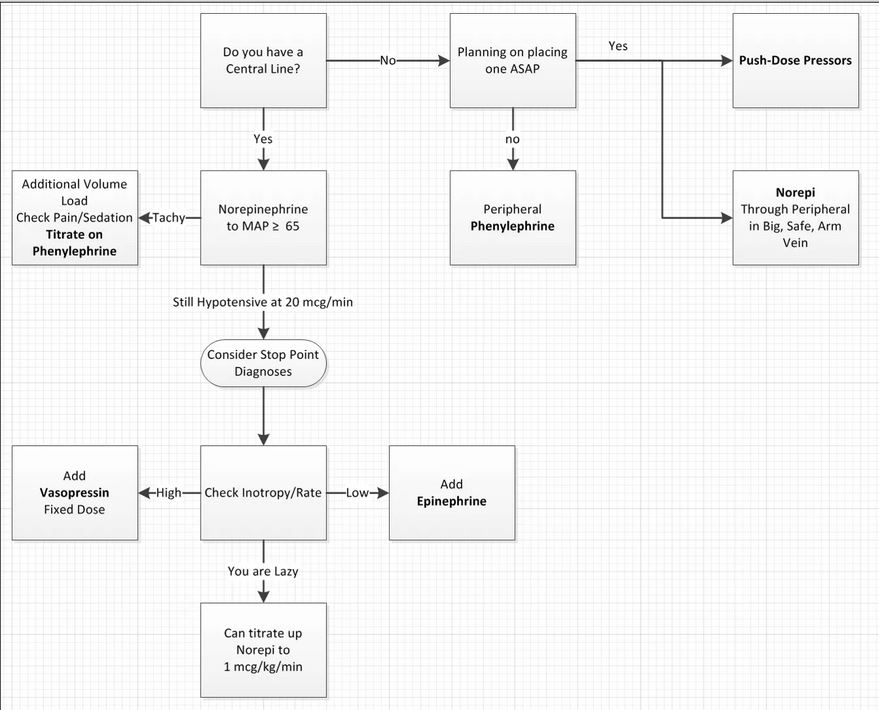
See the Vasopressor Pathway below from Dr. Weingart’s show notes.
Perhaps the most important boxes in this flow chart is for me is:
Be sure to review the podcast below so you know what to do when you get to the stop point box.
See Podcast 87 – Mind of the Resuscitationist: Stop Points [Link to show notes and the podcast] [Critical to Listen to this Podcast] November 26, 2012 by emcrit: “In this Mind of the Resuscitationist Episode, I [Dr. Weingart] discuss stop points: one for when you are using multiple vasopressors and especially about a cognitive stop point whenever things are going south.”
Dr. Weingart suggests a terminology that is clearer than what we have used in the past.
He recommends the term “pure vasopressors” for drugs like phenylephrine and vasopressin
“We should talk about ‘inopressors’ meaning they have both augmentation of cardiac output and heart rate and constriction of the arteries and perhaps veins.”
“And then there are inodilators which we aren’t talking about today [in this lecture].” “The
inodilators are things like dobutamine, milrinone,” and others.
Dr. Weingart states that his first choice as an inopressor for everything except anaphylaxis
is norepinephrine. “It has the most evidence for accomplishing our three goals.”
“It [norepinephrine] has alpha 1 and alpha 2 vasoconstriction; it is arterial and venous side
vasopressor. It has just enough inotropy, I think, to balance things out and make up for any decrease from [increasing] the afterload and [decreasing] the cardiac output by a little push on the beta side.”
You can run norepinephrine peripherally although you shouldn’t do it long term and you want to make sure your IV is good.
“Some of these septic patients need very small doses [of norepinephrine].”
As for dopamine, just don’t use it. It has lots of unfavorable effects.
The clinical markers we use to follow patients are mental status, skin perfusion, and urine
output. And dopamine messes up our ability to follow urine output. Dopamine will cause urine output even if the kidneys are underperfused–and that is bad.
Phenylephrine is a pure vasoconstrictor and has no inotropy and Dr. Weingart sees no useful role for it.
Dr. Weingart used to recommend phenylephrine for push dose pressor. But not any more.
But now he recommends push dose epinephrine for pretty much everything.
Now on to vasopressin. “It is a pure pressor. It does not cause pulmonary vasoconstriction.”
25:31 “The doses we use for things like septic shock, which now is at 0.03 units per minute (it used to be 0.04 units per minute). We put them on a fixed dose. We don’t titrate it. We just leave it there in the background. That dose in a patient who is not vasopressin deficient, doesn’t do anything. And that’s kind of cool. It means it will only be functional, it will only be helpful, in a patient who is sick and has started to chip away at her own endogenous vasopressin.”
“That means that you could always just put it on and if you get an effect you have done something very good for this patient. That means they would have needed massively higher doses of other medicines like catecholamines when all they really needed was to replete a shortage of vasopressin. And if they didn’t need it you are not going to significantly affect their afterload. And your not going to cause much effect. And it means that it is always worth pulling this out of your pocket as you get to higher doses on agents like norepinephrine.”
“And I used to say, you know switch at 20 to adding in vasopressin and retitrating the norepinphrine. And maybe now I’d even do this at a lower dose. And there are some patient populations that you should consider even earlier as the vasopressor. In a future episode we might want to talk about the hemodynamics of massive GI bleeding in a cirrhotic patient. It may be worthwhile to have a background of vasopressin there because it is not going to affect the afterload if they don’t need it. And it will affect the afterload if they did.”
“Suffice it to say that vasopressin is my second-line vasopressor when I think afterload is the problem. And I just add it on to the norepinephrine and see what it does to the norepinephrine dosing and I just do it as a fixed dose. I don’t titrate it. And I have it just hanging around in the background.”
“The last agent I think we will talk about is epinephrine.”
A lot of Dr. Weingart’s friends love epinphrine as their inopressor of choice.
It does cause the lactate to go up via a non anoxic mechanism and so you can’t follow lactate clearance in sepsis. That is not a big deal as the increased lactate levels don’t cause any problems–you just need to know about it.
Based on recent clinical experience, the reason Dr. Weingart does not use epinephrine as his inopressor
“now I like reserving epinephrine as my inotrope. I use epi as an inotrope. I reserve it for purely augmenting what is going on with the heart after I establish my baseline afterload increase with something like norepinephrine. And then I’ll add on the epinephrine to the norepinephrine if I think they now need some additional heart squeezing. Or I might use epinephrine as a single agent, but not in patients whose blood pressure is markedly low. But instead in patients whose blood pressure is okay but the heart is just not doing anything.” [In the Comments section of his show notes he states “. . . for reference, dosing of epi as inotrope in STC CSICU is 0.01-0.08 mcg/kg/min and at this range, rarely saw hyperlactatemia.”]
“And it [the approach above] has really transcended the use of dobutamine for me in most cases. Dobutamine is annoying in that you have to balance the vasodilation with the inotropy.”
“Epinephrine is just nice. It is an inopressor but I reserve it for an inotrope, purely for effecting the heart.”
“When using epinephrine this way, you want to use it in a weight based fashion. And you are using very low doses of epipnephrine, much lower than you would when you are using it for a vasopressor. And therefore I don’t think it effects the lactate very much at all.”
“So except for anaphylaxis, I just grab norepinephrine. If I need additional afterload I add in some vasopressin. If I need additional squeeze on the heart, that is where epinephrine comes to play. And with those three agents, I can do almost anything I need to do with the hemodynamic management of distributive shock or, to some extent, cardiogenic shock as well.”
Comments Section of the Podcast
In the comments section of the podcast, one listener asks:
1. Do you have the fixed dose VPN literature vs titrating the dose (ie if literature even exists)?
2. Do you know if there is literature to show at approximately/ballpark dose epinephrine lactate product begins to overcome the body’s ability to metabolism it ie at what dose does lactic acidosis begin to occur??
And Dr. Weingart replies:
December 3, 2014 at 16:09
1. dose exist. easiest way to find all the refs is to go to SSC guidelines; they have the biblio there.
2. have not seen dose dependent epi/studies; but for reference, dosing of epi as inotrope in STC CSICU is 0.01-0.08 mcg/kg/min and at this range, rarely saw hyperlactatemia.
But all of the comments and responses are thoughtful, helpful, and need to be restudied each time you listen to the podcast. If you are a primary care physician who is only occasionally required to manage patients requiring advanced life support, you can’t listen to the podcast too often and you can’t read all of the comments too often either.
Dr. Mellick’s Vid: Pulse Dose Epi–Intubating the Unstable Patient (Watch and Read!) Posted on January 10, 2014 by Tom Wade MD
Another Great YouTube Video from Dr. Mellick–Pediatric Pulse Dose Pressor Administration Posted on October 2, 2014 by Tom Wade MD
Pulse Dosing of Epinephrine or Phenylephrine for Hypotension
Posted on September 10, 2013 by Tom Wade MD
See Podcast 87 – Mind of the Resuscitationist: Stop Points [Link to show notes and the podcast] [Critical to Listen to this Podcast and read the show n0tes] November 26, 2012 by emcrit: “In this Mind of the Resuscitationist Episode, I [Dr. Weingart] discuss stop points: one for when you are using multiple vasopressors and especially about a cognitive stop point whenever things are going south.”
Bedside Ultrasound in Resuscitation and the Rapid Ultrasound in Shock Protocol Critical Care Research and Practice
Volume 2012, Article ID 503254, 14 pages
Use of Vasoactive Medicines for Septic Shock in Pediatric Advanced Life Support (PALS)
Posted on December 23, 2014 by Tom Wade MD