In this post, I link to and excerpt from Clinical guidelines for the management of treatment-resistant depression: French recommendations from experts, the French Association for Biological Psychiatry and Neuropsychopharmacology and the fondation FondaMental [PubMed Abstract] [Full-Text HTML] [Full-Text PDF]. BMC Psychiatry. 2019 Aug 28;19(1):262.
The above article has been cited by 6 articles in the PubMed Archives.
There are 124 articles similar to the above article in the PubMed Archives.
All that follows is excerpted from the above article.
Definition of resistant depression and at-risk situations
Based on clinical expert consensus, the definition of treatment-resistant depression adopted is the failure of two ADT of adequate duration and dose. The optimal duration is 4 to 6 weeks when the targeted dose is obtained
A history of an unresponsive form of depression is considered the main predictive factor of treatment-resistance and should be meticulously considered. Other potentially predictive indicators are considered, including:
Comorbid anxiety disorder
Comorbid substance abuse
Comorbid personality disorders
Comorbid non-psychiatric chronic and organic disease
The duration of the untreated episode and early or late age at onset of the first depressive episode as well as the illness severity or onset of depression during the peri-menopausal period are recognised as increasing the risk for treatment resistance. Of note, childhood adversity was not explored in our questionnaire, despite it is a well-established prognostic factor for TRD.
Assessments of treatment-resistant depression
The expert panel recommended systematically performing a comprehensive assessment of the depressive episode using the following clinical instruments:
Clinician-rated and self-rated scales of depression severity
Hypomania rating scale
Suicide rating scale
A mood diagram, a structured diagnostic interview as well as a specific questionnaire exploring anxiety disorders can be non-systematically administered.
In cases of depression unresponsive to at least two previous ADT, experts recommended systematically performing the following paraclinical examinations:
Complete blood count, blood electrolytes, liver and renal functions
Lipid profile (cholesterol, triglyceride) and glucose levels
Thyroid-Stimulating Hormone levels (TSHus)
Plasma levels of ADT
Electrocardiogram
Brain MRI
Adjuvant treatments
For patients with anxious features, the adjunctive use of benzodiazepines or hydroxyzine is systematically recommended. The use of buspirone, pregabalin or an ADT belonging to a different pharmacological class is possible in this indication.
The use of an ADT from the same pharmacological class is not recommended.
For patients with sleep disorders, the adjunctive use of hypnotic (zolpidem or zopiclone) is systematically recommended. The use of hydroxyzine, benzodiazepines or an ADT with a different pharmacological profile is possible as an alternative therapeutic option.
For patients with a high risk of self-harm injury, no clear consensus has emerged regarding the use of adjunctive treatment. The experts have suggested several possible options based on the prescription of hydroxyzine, benzodiazepines, second-generation antipsychotics or lithium.
Several treatments are considered as having an antidepressant action:
In monotherapy: bupropion, selective and reversible IMAO-A, quetiapine
In combination with an ADT: lithium, lamotrigine and second-generation antipsychotics
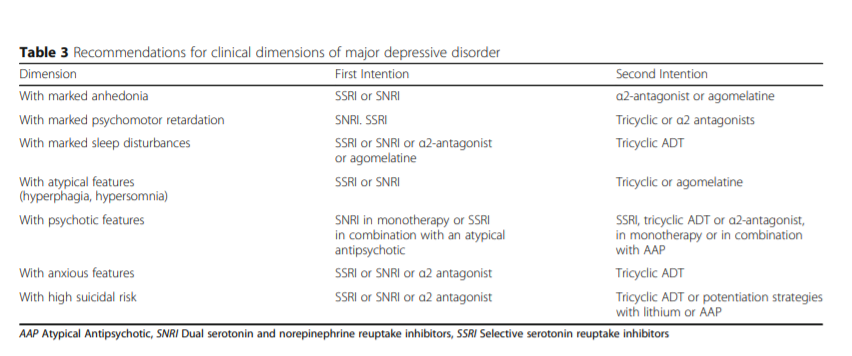
Some clinical characteristics are seen as quality evidence to guide the choice of an ADT, as follows:
For Major Depressive Disorder with a significant aboulia, anhedonia, psychomotor retardation or fatigue: SNRI
For Major Depressive Disorder with a significant weight loss or significant sleep disturbances: α2-antagonist [mirtazapine from Medscape Reference]
For Major Depressive Disorder with a marked depressed mood: tricyclic ADT [see Tricyclic Antidepressants in StatPearls].
Pharmacological strategies in treatment-resistant depression
Switching strategies
Once the decision is made to switch from one ADT to another one, the clinician should consider how this strategy can be implemented. There are three major types of a ADT switch strategies that can be envisaged [13]:
Concurrent switch: changes in the dose of both medications are implemented simultaneously. The new medication is gradually titrated upward while the current agent is gradually tapered downward.
Overlapping switch: dose changes are only implemented for one medication at time, while holding the original medication constant at the original dose until the second medication has reached its optimal dose.
Sequential switch: the dose of the current medication is titrated downward until the interruption. Then, the new medication is introduced.
The concurrent switch is recommended, except when the patient is currently receiving a monoamine oxidase inhibitor (MAOI) medication. In that case, the sequential approach is required during the switching process.
Switching strategies are recommended in the following indications:
No response to the initial treatment
Poor tolerance to the initial treatment
Previous response to the newly introduced treatment
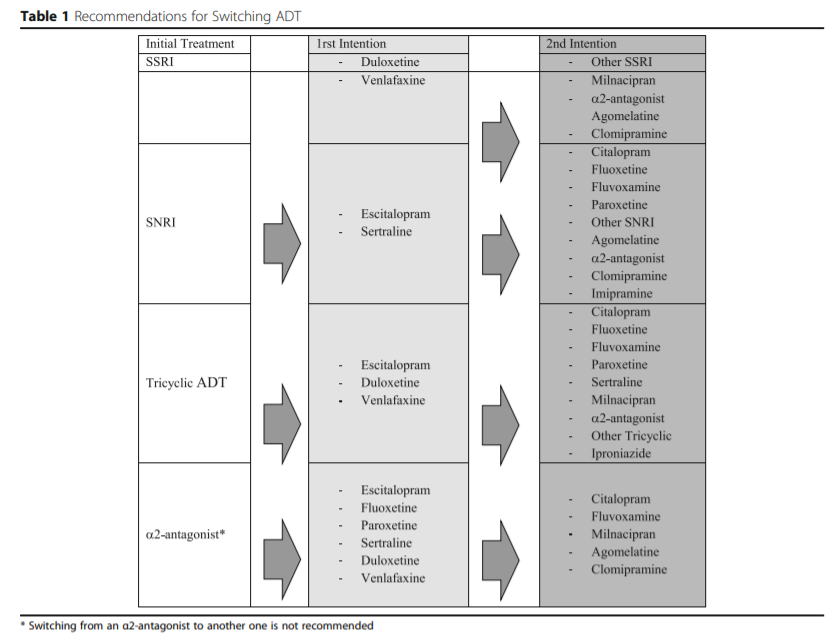
In the first-line, inter-class switch is recommended. The different molecules proposed according to the initial treatment are represented in Table 1.
Combination strategies
The combination strategy (i.e. adding another ADT to an existing one) is only recommended in cases of partial response, after 4 to 6 weeks of adequate treatment. In the first-line treatment, the recommended strategies consist of the following combinations:
SSRI + α2 antagonist
SNRI + α2 antagonist
Tricyclic ADT + α2-antagonist
The recommended doses range from 15 to 30 mg per day for mirtazapine and 30 to 60 mg per day for mianserine [mianserine is not available in the U.S]. In the second-line treatment, an association between SSRIs, SNRIs or tricyclic ADT and agomelatine can be proposed. The maintenance of the combined ADT is recommended for a period of six months once clinical remission is obtained. A period of one year is not justified, except in specific indications.
Add-on strategies
The potentiation strategy is only recommended in cases of partial response, after 4 to 6 weeks of adequate treatment. Adding lithium or quetiapine to the ongoing ADT is recommended to enhance ADT efficacy (Table 2). The use of thyroid hormones or aripiprazole is proposed as a second intention. In this indication, second-generation antipsychotics such as risperidone, olanzapine, clozapine, amisulpride) or anticonvulsants (apart from lamotrigine) are not recommended.
Thyroid hormone supplementation is recommended in combination with SNRIs or tricyclic ADT, and eventually with SSRIs or α2-antagonists. No consensus could be reached regarding the targeted doses, but the dose typically used for this purpose is 25 to 50 μg/day of L-T3. A pre-therapeutic assessment is recommended and includes:
Physical examination
Electrocardiogram
Determination of Thyroid-Stimulating Hormone levels
In the absence of a consensus, the targeted dose should allow TSH levels ranging from 0.1 to 1 μg/L to be achieved.
Organisation of sequenced treatment
First-line strategy
Two main criteria were proposed to the experts that could guide the selection of the appropriate therapeutic strategy: the intensity of the current depressive episode and associated clinical features.
Recommendations for mild, moderate and severe depression
SSRIs and SNRIs are considered a first-line treatment, regardless of the clinical severity, without distinguishing between these types of ADT.
For severe depression, psychotherapies are only recommended in combination with ADT, whereas they can be proposed in monotherapy in mild to moderate major depressive episodes.
Tricyclic ADT, α2-antagonists or agomelatine can be proposed as a second-line treatment in severe depression.
No clinical features support the use of different ADT in combination in first-line.
Second-, third-, fourth-, fifth- and sixth-line strategies
Start here