In this post I link to and excerpt from Emergency Medicine Cases‘ Ep 175 Emergency Orthopedics Differential: SCARED OF Mnemonic – When X-rays Lie*, October, 2022.
*Helman, A. Chadha, Y. Sayal, A. Emergency Orthopedics Differential: SCARED OF Mnemonic. Emergency Medicine Cases. October, 2022. https://emergencymedicinecases.com/orthopedics-differential-scared-of-mnemonic. Accessed October 30, 2022.
All that follows is from the above resource’s outstanding show notes.
In this main episode podcast, Dr. Arun Sayal creator of the CASTED course and Dr. Yatin Chadha a radiologist with a fellowship in MSK radiology, join Anton for Part 1 of 2 podcasts on Emergency Orthopedic Injuries. This episode focuses on a differential diagnosis of MSK injuries that are occult to X-ray with the help of the SCARED OF mnemonic. It ensures we pick up all the “can’t miss” diagnoses that can be easily overlooked when we do not integrate a pointed history and physical exam with the X-ray in front of us. Essentially, we discuss ‘when X-rays lie’ and offer up a variety of clinical pearls and pitfalls in assessing patients in the ED with MSK presentations…
The occult MSK X-ray: A normal X-ray does not preclude serious pathology
Just as a normal ECG does not rule out ACS, a normal x-ray does not rule out all serious MSK pathology. We tend to over-rely on x-rays to diagnose orthopedic injuries, sometimes overlooking key historical and physical exam data points that should inform our pre-test probability. As in all ED presentations, we should apply Bayesian analysis to orthopedic cases.
Using history to inform our pre-test probability for MSK pathology
Important aspects in history taking for MSK presentations that may influence pre-test probability:
- Age (certain fractures tend to occur in specific age ranges e.g. scaphoid fractures have peak incidence age 20-29)
- Traumatic/atraumatic mechanism
- Previous injuries
- Past medical history (e.g. cancer/autoimmune disease/other immunocompromising disease, osteoporosis)
- Medications (e.g. steroids/immunosuppressants – risk factors for septic arthritis, medications for osteoporosis)
Dr. Sayal’s SCARED OF mnemonic: An approach to orthopedic differential diagnosis
In the presence of a normal (or near-normal) X-ray, what should we be “scared of”?
1. Septic arthritis
For patients who present with non-traumatic MSK pain, infection including septic arthritis/bursitis, osteomyelitis and discitis and should be near the top of the differential diagnosis.
The accuracy (or inaccuracy) of lab tests for septic arthritis
__________________________________________________________
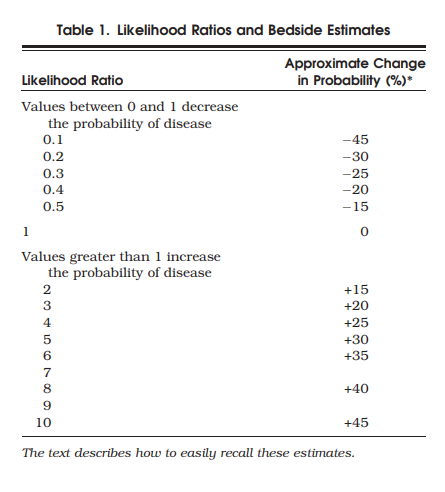
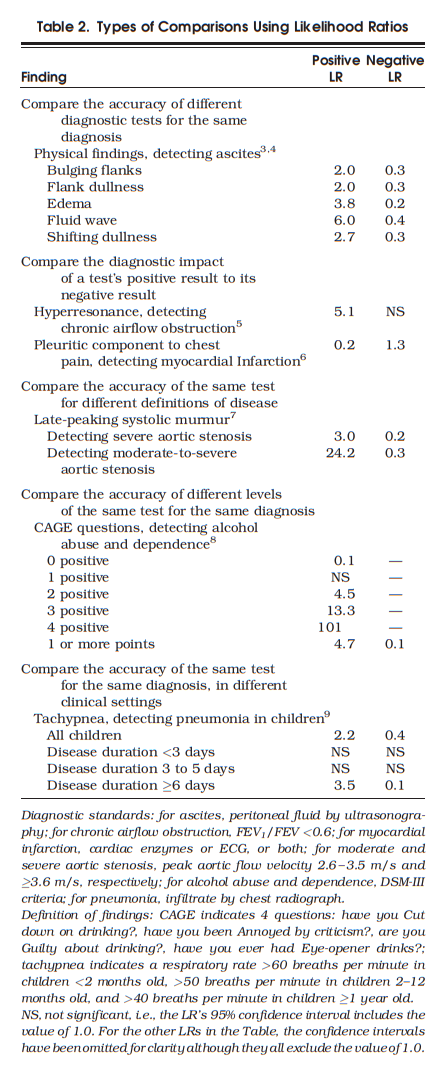
*Likelihood ratios: Please see Likelihood Ratios – Some Resources With Excerpts
Posted on November 20, 2018, by Tom Wade MD [Note to myself: This link is a good quick review of how to use likelihood ratios.
*See also The NNT:
- Quick summaries of evidence-based medicine.
“We are a group of physicians that have developed a framework and rating system to evaluate therapies based on their patient-important benefits and harms as well as a system to evaluate diagnostics by patient sign, symptom, lab test or study.” - Diagnosis (LR) Reviews
“You’ll find all of our diagnostic/likelihood ratio reviews, arranged by medical specialty, organ system, and alphabetically.”
See also Simplifying Likelihood Ratios [PubMed Abstract] [Full Text HTML] [Full Text PDF].J Gen Intern Med. 2002 Aug; 17(8): 647–650.
____________________________________________________________
The likelihood ratios for serum tests are variable across studies and do not appear to be very predictive, especially in immunocompromised patients. In one review “no cutoff for ESR or CRP significantly increases or decreases the post-test probability of septic arthritis.”
- ESR > 20mm/hr +LR 0.84, -LR 2.4
- ESR > 30mm/hr +LR 1.3, -LR 0.17
- ESR > 50mm/hr +LR 1.4, -LR 0.4
- ESR >100mm/hr +LR 7.0, -LR 0.6
- CRP >10 mg/L +LR 1.1-1.4, -LR 0.3-0.6
- CRP >100mg/L +LR 1.1-2.8, -LR 0.3-0.6
Synovial fluid tests likelihood ratios
Without testing synovial lactate levels, synovial fluid analysis had an overall sensitivity of only 70-80% which drops to 50% when antibiotics are administered prior to the arthocentesis. However when synovial lactate is included, synovial fluid analysis has excellent test characteristics for the diagnosis of septic arthritis. Tissue culture is the gold standard diagnostic test for septic arthritis.
Synovial PMNs >90% +LR 2.7, -LR 0.51
Synovial lactate >5.6 mmol/L +LR 2.4, -LR 0.46
Synovial lactate >12 mmol/L +LR 19, -LR 0.16
Pearl: Synovial fluid lactate has demonstrated excellent diagnostic accuracy for septic arthritis with +LRs as high as 19 and -LR as low as 0.16.
Pitfall: Synovial fluid analysis overall has a 70-80% sensitivity and antibiotics prior to the tap can drop sensitivity by up to 50%!
In patients with septic arthritis, while some large joints such as the knee often are visibly swollen and relatively easy to access for fluid aspiration, other large joints such as the hip rarely appear visibly swollen, usually require fluoroscopy-guided aspiration and so imaging may be more often used to help support a diagnosis of septic arthritis.
X-ray findings in septic arthritis: Often overlooked, and if present should increase suspicion
While the x-ray is usually normal in patients with septic arthritis (especially in early presenters), the following findings should increase one’s suspicion for septic arthritis.
- Effacement of fat planes lateral to the hip joint: lateral to the hip joint there are 3 bands of soft tissue (rectus femoris, gluteus minimus and gluteus medius); effacement of the low density strips in between these bands of soft tissue compared to the contralateral side suggest a joint effusion which increases the likelihood of septic arthritis in a patient with non-traumatic hip pain
- Joint space narrowing: joint space narrowing compared to the contralateral side and compared to previous imaging when available
- Bony erosions
See also Normal radiographic anatomy of the hip from Radiopaedia.
Ultrasound, CT and MRI in the diagnosis of septic arthritis
- While a joint effusion found on ultrasound increases the likelihood of septic arthritis in patients where you have a suspicion, a negative ultrasound for effusion does not rule out septic arthritis.
- Although CT is generally very accurate at detecting fractures that are occult to x-ray, they are inaccurate for the diagnosis of septic arthritis, and are not the preferred advanced imaging modality of choice according to our experts.
- MRI is the advanced imaging modality of choice for patients suspected of septic arthritis in whom a joint aspiration is not possible or unsuccessful.
Pitfall: A common pitfall is to rule out septic arthritis of the hip if an ultrasound is negative for joint effusion. A negative ultrasound for effusion does not rule out septic arthritis: because the ultrasound of the hip is performed on a supine patient, and fluid collects in the dependent portion of the joint, an effusion may not be seen when evaluating the hip anteriorly.
2. Compartment Syndrome: Forget about the 6 Ps (except for board exams) and yes, it can occur after trauma without fracture
Start here.