I’ve divided these posts, my study notes on the European high blood pressure guidelines, into several parts for ease of my review:
- Here is the link to Diagnosis of Hypertension-Part 1 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
Posted on November 10, 2019 by Tom Wade MD - This post Treatment of Hypertension-Part 2 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
Posted on November 15, 2019 by Tom Wade MD - Here is the link to The Drug Treatment Algorithm For Hypertension – Part 3 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
Posted on November 16, 2019 by Tom Wade MD - Here is the link to Hypertension In Specific Circumstances – Part 4 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
Posted on November 16, 2019 by Tom Wade MD
There are links to additional resources after this post.
The following are Therapy Excerpts from the 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/ehy339:
7.1 Beneficial effects of blood pressure lowering therapy in hypertension
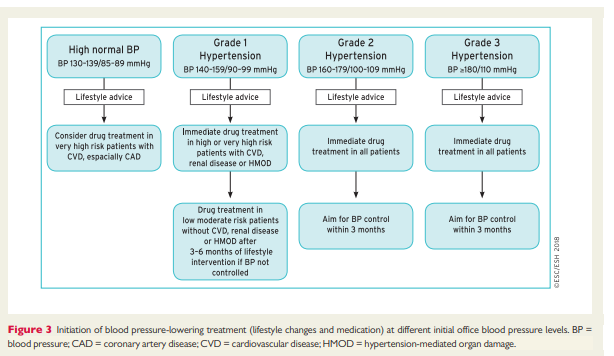
There are two well-established strategies to lower BP: lifestyle interventions and drug treatment. Device-based therapy is also emerging, but is not yet proven as an effective treatment option. Lifestyle interventions can undoubtedly lower BP and in some cases CV risk (see section 7.4.1), but most patients with hypertension will also require drug treatment. The drug treatment of hypertension is founded on very solid evidence, underpinned by the largest number of outcome based RCTs in clinical medicine. Meta-analyses of RCTs including several hundred thousand patients have shown that a 10 mmHg
reduction in SBP or a 5 mmHg reduction in DBP is associated with significant reductions in all major CV events by 20%, all-cause mortality by 10 – 15%, stroke by 35%, coronary events by 20%, and heart failure by 40%.2,8 These relative risk reductions are consistent, irrespective of baseline BP within the hypertensive range, the level of CV risk, comorbidities (e.g. diabetes and CKD), age, sex, and ethnicity.2,201Relative outcome reductions calculated by two recent metaanalyses are similar to those provided by the original meta-analysis of the effects of BP lowering on outcomes in 1994.202 Thus, the benefits of antihypertensive treatment have not been attenuated by the widespread concomitant prescription of lipid-lowering and antiplatelet therapies in contemporary medicine.
Another important objective of antihypertensive therapy is to
reduce the development of CKD; however, the slow rate of decline in renal function in most hypertensive patients makes the demonstration of potential benefits of BP lowering difficult. Consequently, the protective effect of BP reduction on kidney function can be less obvious and has been restricted to patients with diabetes or CKD, in whom there is a faster rate of disease progression.203 Some, but not all, RCTs have also shown a protective effective of BP lowering on the progression of CKD towards end-stage renal disease in both diabetic and non-diabetic nephropathy.
7.3.1 New evidence on systolic blood pressure and diastolic blood pressure treatment targets
Whilst considering BP targets, it is important to acknowledge that <50% of patients treated for hypertension currently achieve a target office SBP of <140 mmHg.11,12 This is a major missed opportunity forCVD prevention in millions of people across the world.
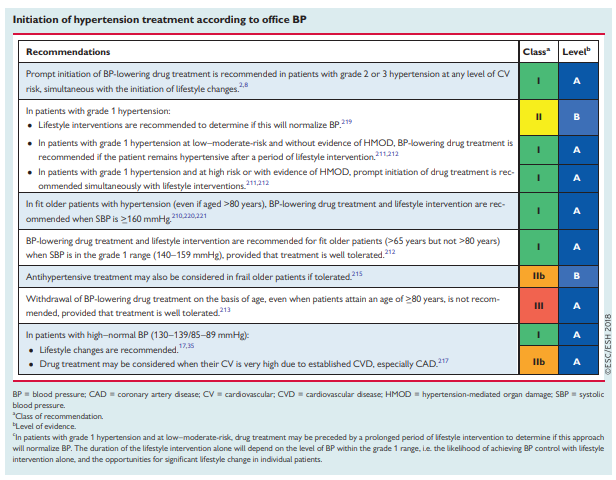
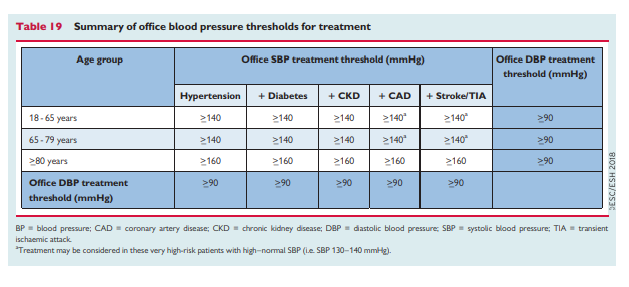
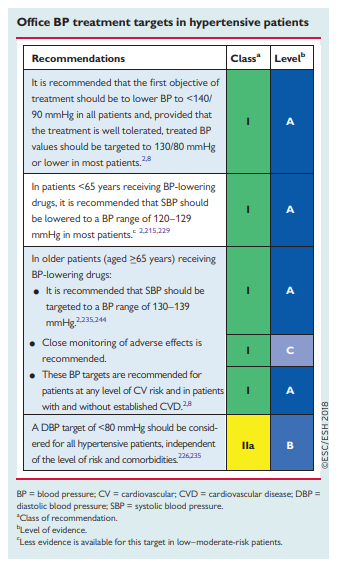
This Task Force recommends that when BP-lowering drugs are
used, the first objective should be to lower BP to <140/90 mmHg in all patients. Provided that the treatment is well tolerated, treated BP values should be targeted to 130/80 mmHg or lower in most patients, although in some groups the evidence is less compelling. In older patients (>65 years), SBP should be targeted to between 130 and 140 mmHg, and DPB to <80 mmHg. Treated SBP should not be targeted to <120 mmHg.Importantly, we specify a target range because the lower safety
boundary assumes greater importance when BP is targeted to lower levels. Furthermore, in general, when SBP is lowered to <120 mmHg in patients included in RCTs (i.e. older and higher-risk patients, often with comorbidities and CVD), the risk of harm appears to increase and outweigh the benefits.2227.3.2.1. Diabetes mellitus
RCTs in type 1 diabetes mellitus demonstrate that BP-lowering treatment has a renoprotective effect,228 but because these patients tend to be younger, previous RCTs have had inadequate power to study CV outcomes and to establish optimal BP targets.
In contrast, there have been many BP-lowering treatment RCTs,
either exclusively dedicated to patients with type 2 diabetes or
hypertension trials that have included a large cohort of patients with type 2 diabetes.2 Most of these RCTs have shown that BP lowering to <140/85 mmHg is beneficial in patients with type 2 diabetes and hypertension. However, the results have been less clear about whether a lower BP target is associated with further benefits.
The article summarizes, on p 3052 of the PDF, seven articles and concludes:
In summary, In patients with diabetes receiving BP-lowering drugs, it is recommended that office BP should be targeted to an SBP of 130 mmHg,229 and lower if tolerated. In older patients (aged >_65 years) the SBP target range should be 130–140 mmHg213 if tolerated. SBP should not be lowered to <120 mmHg and DBP should be lowered to <80 mmHg. Attention should also be given to the consistency of BP control, because visit-to-visit BP variability is associated with increased CV and renal disease risk. Furthermore, CV protection has been found to be greater when BP control is accompanied by fewer visit-to-visit BP variations.239–241
7.3.2.2. Older patients
The definition of ‘older’ is complex. As populations age, there is
increasingly wide variation between a patient’s chronological age and their functional status, ranging from fit, active, and independent, through to frail* and dependent. The anticipated benefits vs. potential harm of BP treatment in older patients will be influenced by the patient’s ability to tolerate treatment and their health and functional status. For the purposes of these Guidelines, ‘older’ patients are defined as those aged >_65 years.[The article summarizes the new data on p 3053 of the PDF]
*Note to myself: Both sets of links below need their own posts sometime in the NEAR future.
*Here are links to two articles on frailty:
- The Frailty Syndrome: Definition and Natural History [PubMed Abstract]. Clin Geriatr Med. 2011 Feb;27(1):1-15.
- Frailty in elderly people [PubMed Abstract]. Lancet. 2013 Mar 2;381(9868):752-62
*And here are links on The Comprehensive Geriatric Assessment:
- Comprehensive geriatric assessment – a guide for the non-specialist [PubMed Abstract]. Int J Clin Pract. 2014 Mar;68(3):290-3
- What is Comprehensive Geriatric Assessment (CGA)? An umbrella review [PubMed Abstract]. Age Ageing. 2018 Jan 1;47(1):149-155.
- RESOURCES for the COMPREHENSIVE GERIATRIC ASSESSMENT based PROACTIVE PERSONALISED PRIMARY CARE of the ELDERLY
- This is an awesome site that should be carefully reviewed by all primary care clinicians. The site won the 2018 Irish Healthcare Award:
Innovative GP Project of the Year: An award for outstanding work in the form of improvements or innovations implemented by individuals in a general practice setting, at either a clinical or practice management level, that improves the quality of patient care or helps free up GP time
Resuming excerpts from Treatment of Hypertension-Part 2 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
7.3.2.2. Older patients (Continued from above)
[The article summarizes the new data on p 3053 of the PDF]
Based on the new data, the targets suggested by the previous
Guidelines now appear too conservative for many old and very old patients, especially those who are active and independent.
Consequently, we recommend that in older patients treated for
hypertension, BP should be lowered to <140/80 mmHg, but not
below an SBP of 130 mmHg. Importantly, the impact of BP-lowering on the well-being of the patient should be closely monitored, because the increased risk of adverse events (e.g. injurious falls) with lower BP values could be more pronounced in older patients in the real-life setting than in the closely monitored conditions of RCTs. Further details on the approach to treatment of the frail older patient are discussed in section 8.8.7.3.2.3 Office vs. home and ambulatory blood pressure targets
No outcome-based RCT has used ABPM or HBPM to guide the
treatment of hypertension. Thus, ABPM and HBPM BP targets are based on extrapolation from observational data rather than on outcome trials. Although we do not provide formal ABPM or HBPM BP targets for treated patients, it should be noted that:(1) In population studies, the difference between office and out-of office BP levels decreases as office BP decreases, to a point of
around 115 – 120/70 mmHg, at which office and 24 h ABPM mean BP values are usually similar.54
(2) This convergence has also been confirmed in treated patients243 in whom the difference between office BP and ambulatory BP values diminishes and becomes negligible at an SBP of approximately 120 mmHg.
(3) In treated patients, a target office SBP of 130 mmHg might therefore correspond to a slightly lower mean 24 h SBP, i.e. approximately 125 mmHg. (4) Although there are no available data, the home SBP target, to be equivalent to an office SBP target of 130 mmHg, might also be lower than 130 mmHg
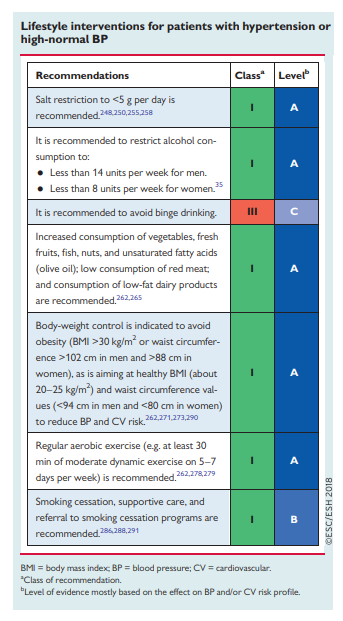
7.4.1 Lifestyle changes
7.5. Pharmacological therapy for hypertension
7.5.1 Drugs for the treatment of hypertension
Most patients will require drug therapy in addition to lifestyle measures to achieve optimal BP control. In the previous Guidelines, five major drug classes were recommended for the treatment of hypertension: ACE inhibitors, ARBs, beta-blockers, CCBs, and diuretics (thiazides and thiazide-like diuretics such as chlortalidone and indapamide), based on: (i) proven ability to reduce BP; (ii) evidence from
placebo-controlled studies that they reduce CV events; and (iii) evidence of broad equivalence on overall CV morbidity and mortality, with the conclusion that benefit from their use predominantly derives from BP lowering. These conclusions have since been confirmed by recent meta-analyses.1,2,217,292 These meta-analyses have reported cause-specific differences on outcomes between some drugs (e.g. less stroke prevention with beta-blockers, and less heart failure prevention with CCBs); however, overall, major CV outcomes and mortality were similar with treatment based on initial therapy with all five major classes of treatment. These Guidelines thus recommend that the same five major classes of drugs should form the basis of antihypertensive therapy. There are compelling or possible contraindications for each class of drug (Table 20) and preferential use of some drugs for some conditions, as discussed below. There is also evidence that there are differences in the persistence and discontinuation rates of the major drug classes.293,294
Other classes of drugs have been less widely studied in eventbased RCTs or are known to be associated with a higher risk of adverse effects [e.g. alpha-blockers, centrally acting agents, and mineralocorticoid receptor antagonists (MRAs)]. These are useful additions to the antihypertensive armamentarium in patients whose BP cannot be controlled by proven combinations of the aforementioned major drug classes.
7.5.2 Drug treatment strategy for hypertension
Guidelines have generated a variety of different strategies to initiate and escalate BP-lowering medication to improve BP control rates. In previous Guidelines, the emphasis was on initial use of different monotherapies, increasing their dose, or substituting for another monotherapy. However, increasing the dose of monotherapy produces little additional BP lowering and may increase the risk of adverse effects, whilst switching from one monotherapy to another is frustrating, time consuming, and often ineffective.
For these reasons, more recent Guidelines have increasingly focused on the steppedcare approach, initiating treatment with different monotherapies and then sequentially adding other drugs until BP control is achieved. Despite this, BP control rates have remained poor worldwide.
[Few hypertensive patients reach goal. So what we are currently doing needs to change what we are doing.]
This Task Force believes that one of the most important issues to address in these Guidelines is ‘how do we improve BP control in treated patients?’. This has become an even more pressing matter because, based on new evidence, current Guidelines are recommending more stringent BP targets (on-treatment values of <_ 130/80 mmHg in the general population and <_ 140/90mm Hg in older hypertensive people), which will make the achievement of BP control even more challenging.
[On p 3059 of the Guidelines PDF, the authors suggest why we are failing to get the desired blood pressure control.]
The above considerations suggest that the most effective
evidence-based treatment strategy to improve BP control is one that: (i) encourages the use of combination treatment in most patients, especially in the context of lower BP targets; (ii) enables the use of SPC (single pill combination) therapy for most patients, to improve adherence to treatment; and (iii) follows a treatment algorithm that is simple, applies to all patients, and is pragmatic, with the use of SPC therapy as initial therapy for most patients, except those with BP in the high–normal range and in frail older patients (see below).7.5.2.1. Drug combinations for hypertension treatment
Based on the results of outcome RCTs and recent meta-analyses,
and evidence of BP-lowering effectiveness, all five major drug classes can, in principle, be combined with one another, except for ACE inhibitors and ARBs, whose concomitant use may lead to no additional benefit but increased adverse effects and is thus discouraged.We recommend that the treatment of hypertension should be preferentially based on combinations of an ACE inhibitor or ARB with a CCB and/or a thiazide/thiazide-like diuretic. These combinations are now widely available in a single pill and in a range of doses, facilitating simplification of treatment, flexible prescribing, and uptitration from lower to higher doses. Combination therapy that includes an ACE
inhibitor or ARB with either a CCB or thiazide/thiazide-like diuretic are complementary because both CCBs or diuretics activate the RAS, which will be counteracted by their combination with an ACE inhibitor or ARB. These combinations will also limit potential adverse effects associated with diuretic or CCB monotherapy, reducing the
risk of hypokalaemia due to diuretics and reducing the prevalence of peripheral oedema due to CCBs. These combinations also ensure that the RAS is inhibited as part of the treatment strategy, which is an important consideration for many patient groups (e.g. diabetes, LVH, proteinuria).
7.5.2.2 Rationale for initial two-drug combination therapy for most patients
As discussed above and with the emphasis in these Guidelines on
achieving a BP target in most patients of <130/80 mmHg, the majority of patients will require combination therapy. Initial combination therapy is invariably more effective at BP lowering than monotherapy, indeed even low-dose combination therapy is usually more effective than maximal dose monotherapy.341 Furthermore, the combination of medications targeting multiple mechanisms, such as blocking the RAS as well as inducing vasodilatation and/or diuresis, reduces the heterogeneity of the BP response to initial treatment and provides a steeper dose response than is observed with escalating doses of monotherapy.342 Finally, two-drug combinations as initial therapy have been shown to be safe and well tolerated, with no or only a small increase in the risk of hypotensive episodes,341 even when given to patients with grade 1 hypertension,343 in which adverse events leading to treatment discontinuation are infrequent.2947.5.2.3 Uptitration of treatment to three-drug combination therapy
Studies suggest that two-drug combination therapy will control BP in approximately two-thirds of patients.341
For patients whose BP is not controlled by two-drug combination therapy, the logical option is to increase treatment to three-drug combination therapy: usually a RAS blocker, a CCB, and a diuretic.
Studies suggest that a three-drug combination should control BP in >80% of patients.349,350 This rate of BP control is much greater than the current rate of BP control across Europe in treated hypertensive patients. We do not recommend three-drug combinations as initial therapy.
7.5.2.5 Further uptitration of antihypertensive therapy
When BP remains uncontrolled with three-drug combination therapy, the patient is classified as having resistant hypertension, assuming that secondary causes of hypertension and poor adherence to treatment have been excluded, and that the elevation in BP has been confirmed by repeated office BP measurement, ABPM, or HBPM (see section 8.1). Such patients should be considered for specialist evaluation.
Additional treatment options include the addition of low-dose spironolactone (25 – 50 mg daily)310 or another additional diuretic therapy [higherdose amiloride 10 – 20 mg daily,357 higher dose thiazide or thiazide-like diuretics, loop diuretics in patients with significant renal impairment (eGFR <45 mL/min/m2), beta-blockers, alpha-blockers, centrally acting
agents (e.g. clonidine), or, rarely, minoxidil] (see section 8.1)
And now go on to
The Drug Treatment Algorithm For Hypertension – Part 3 Of Links To And Excerpts From The 2018 European Guidelines For The Management Of Hypertension
Posted on November 16, 2019 by Tom Wade MD
Resources:
(1) 2018 ESC/ESH Guidelines for the management of arterial hypertension [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Eur Heart J. 2018 Sep 1;39(33):3021-3104. doi: 10.1093/eurheartj/.
(2) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. [PubMed Citation] [Full Text PDF]. Hypertension. 2018 Jun;71(6):1269-1324. doi: 10.1161/HYP.0000000000000066. Epub 2017 Nov 13.
(3) Screening for Endocrine Hypertension: An Endocrine Society Scientific Statement [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Endocrine Reviews, Volume 38, Issue 2, 1 April 2017, Pages 103–122
(4) 2016 European Guidelines on cardiovascular disease prevention in clinical practice [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Atherosclerosis. 2016 Sep;252:207-274. doi: 10.1016/j.atherosclerosis.2016.05.037.
(5) “HOW TO CHECK A HOME BLOOD PRESSURE MONITOR FOR ACCURACY” From The American Medical Association
Posted on November 14, 2019 by Tom Wade MD