The following is from reference (1):
Asthma presents with recurrent episodes of wheezing, dyspnea, prolonged expiratory phase, and diminished air exchange secondary to narrowing of midsized and small airways. This leads to increased work of breathing with chest retractions, hypoxia (low oxygen saturation less than 93%) and poor feeding. Status asthmaticus exists when there is a failure to respond to initial bronchodilator therapy.
Severe asthma: marked chest tightness, marked wheezing and retractions, cyanosis and inability to speak in sentences, hunched posture, and altered mental status.
Assessment:
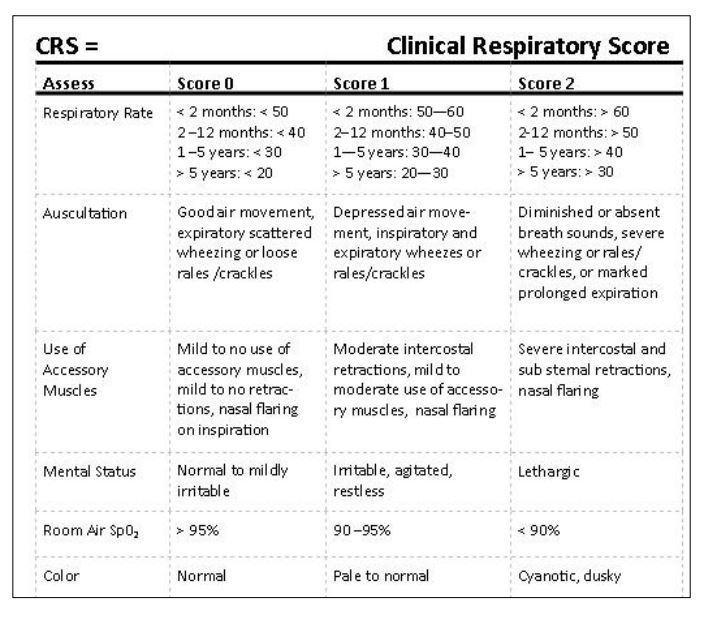
ABC’s-vital signs and pulse oximetry – – circulatory respiratory status characterize the degree of respiratory distress (Clinical Respiratory Score*)
Respond appropriately per BLS/PALS protocols
Onset of symptoms, current medications, risk factors for severe disease (below)
Management:
Oxygen:
Administer oxygen to maintain SpO2 to greater than or equal to 92%.
Nasal cannula, blow by oxygen, facemask at 5 L per minute or
Non-rebreather oxygen mask at greater than 10 L per minute
Nebulized bronchodilators:
Albuterol 0.15 mg per kilogram (minimum 2.5 mg; maximum: 5 mg) In combination with Ipratropium (0.25 mg: less than 12 years; 0.5 mg: greater than 12 years)
May repeat every 20 min. for three doses
or
Short acting Beta agonist (albuterol MDI) with valved spacer
If mild: less than two years: 4 puffs; greater than or equal to two years: 6 puffs 1 dose and reassess
If worse: less than two years: 6 puffs; greater than two years: 6 – 8 puffs Q 20 min. up to three doses
If poor air entry and patient unable to cooperate, may administer 1:1000 epinephrine 0.01 mL per kilogram SC (max: 0.3 mL)
Steroids
Administer PO prednisolone 2 mg per kilogram ASAP (max: 60 mg) or PO or IM dexamethasone 0.2 mg per kilogram (Max: 10 mg)
Caution in cases with potential life-threatening asthma:
- Previous intubation or ICU admission.
- Greater than or equal to two hospitalizations or greater than or equal to 3 ED visits in the past year.
- Use of greater than 1 canister of short acting Beta agonist per month.
- Poor compliance and access to care.
- Lack of perception of disease severity (parent or child).
- Rapid disease progression.
- Major psychosocial problems.
Transfer to ED/call EMS when
- No improvement in initial three bronchodilator treatments.
- Persisting low oxygen saturation (less than 94%)
- Marked increase work of breathing and exhaustion.
- Poor mental status – – somnolence, agitation, lethargy
*Clinical Respiratory Score (CRS) in asthma exacerbations:
Mild exacerbation: CRS: less than or equal to 3
Moderate exacerbation: CRS: 4–6
Severe Exacerbation: CRS: 6–8
Resources:
(1) The Complete Resource on Pediatric Office Emergency Preparedness. 2013. Springer. This excellent book is brief and to the point. The authors are from Texas Children’s Hospitaland Texas Children’s Pediatrics. Asthma, pp 17 + 18.