In this post, I review and excerpt from The Cribsiders‘ IDENTIFYING AND MANAGING MILD TRAUMATIC BRAIN INJURY IN CHILDREN, FEBRUARY 17, 2021 By JUSTIN BERK.*
*Kelly JM, Lumba-Brown A, Chui C, Berk J. “Concussion: The Diagnosis and Management of Mild Traumatic Brain Injury in Children”. The Cribsiders Pediatric Podcast. https:/www.thecribsiders.com/ February, 2021.
All that follows is from the above outstanding resource.
Summary
Jump into pediatric mild traumatic brain injury with our guest, Dr. Angela Lumba Brown, a pediatric emergency medicine physician and Associate Professor of Emergency Medicine, Pediatrics, and Neurosurgery at Stanford University. In this episode, we talk about the diagnosis of mild traumatic brain injury, when to get neuroimaging for head trauma, and the five concussion subtypes. We also discuss how you can support your patients in their recovery to get them back to their daily activities and what disparities exist in head trauma. Join us to have your mind blown with this fascinating topic.
Concussion Pearls
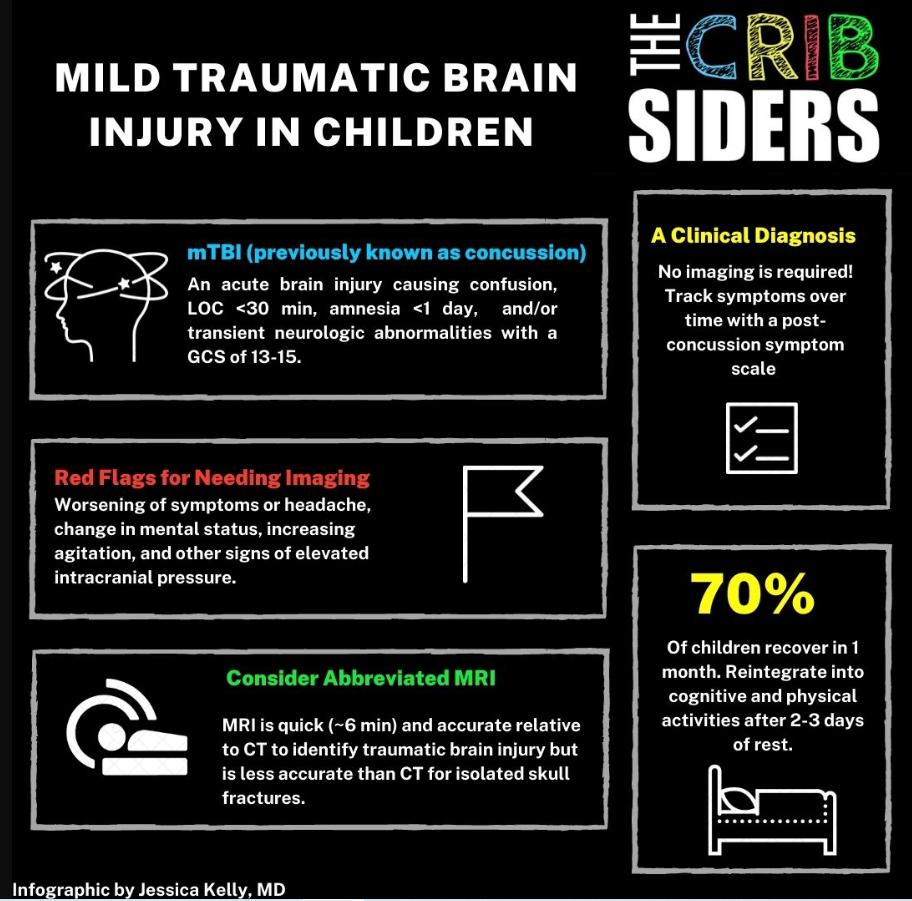
- The term mild traumatic brain injury (mTBI) is used to describe an acute brain injury that results in confusion, loss of consciousness, amnesia, and/or transient neurological findings with a GCS of 13-15
- mTBI is a clinical diagnosis and does not require neuroimaging to diagnose
- Several clinical decision making tools are available to help clinicians identify patients at risk for severe head injuries who need neuroimaging versus patients who can be safely observed
- Abbreviated MRI can be used in the diagnosis of traumatic brain injury
- Patients with worsening of symptoms or headache, change in mental status, increasing agitation, or signs of elevated intracranial pressure should receive neuroimaging
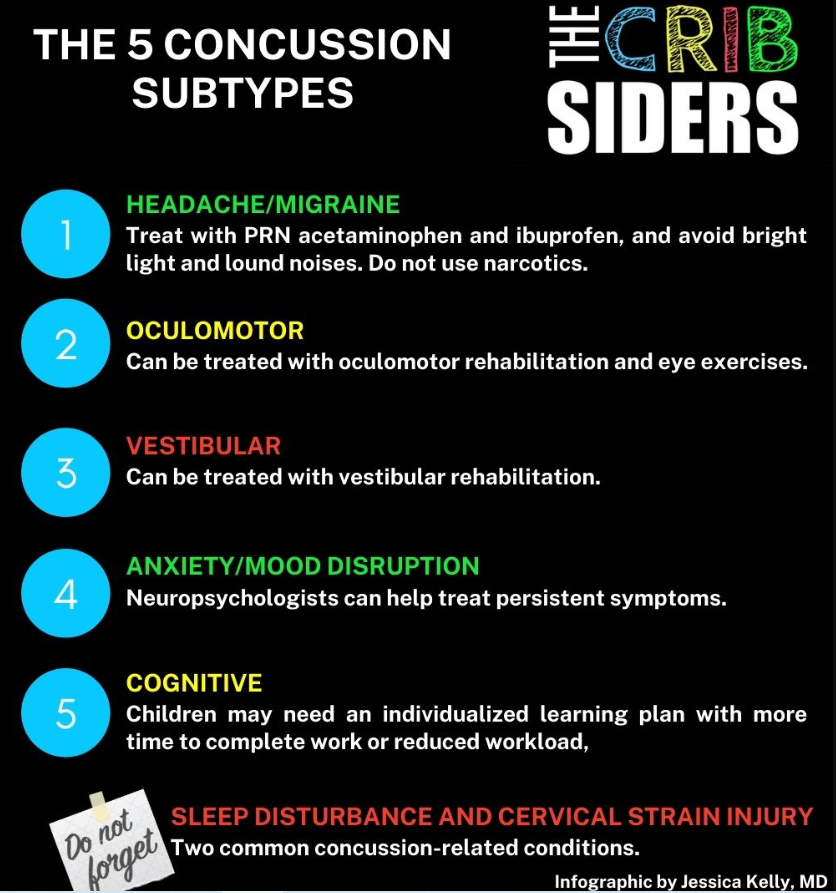
- The five concussion subtypes are headache/migraine, oculomotor, vestibular, anxiety/mood, and cognitive, and each of these subtypes should be addressed and treated by providers if present
Concussion Notes
Dr. Angela Lumba Brown talks to us about mild traumatic brain injury (mTBI) in children.
Mild Traumatic Brain Injury (mTBI)
- Use the term mTBI rather than concussion or minor head injury (Lumba-Brown et al. JAMA Pediatr. 2018). These terms have been used interchangeably in the past but have different connotations for families, researchers, and clinicians which can lead to misinterpretation
- mTBI is an acute brain injury resulting from mechanical injury to the head or from external forces resulting in confusion/disorientation, loss of consciousness <30 min, post-traumatic amnesia <1 day, and/or transient neurologic abnormalities (focal signs or seizures) with a GCS of 13-15.
- mTBI is a clinical definition and does not require neuroimaging to diagnose
- After head trauma, children may have headache, nausea, emesis, dizziness, difficulty with concentrating or sleeping, and/or anxiety or mood disruption
- Symptoms depend on many factors, including premorbid factors (PMHx, psychiatric history, propensity for mTBI) and the injury itself
- Complicated mTBI: mTBI plus swelling, intracranial bleeding, microhemorrhage, or contusion on neuroimaging
IMAGING IN MTBI
- Neuroimaging is not needed to diagnose mTBI in a child
- Several decision making rules guide the choice to obtain head CT when concerned for severe head injury depending on risk factors: the Pediatric Emergency Care Applied Research Network (PECARN) clinical prediction tool, the Children’s Head injury ALgorithm for the prediction of Important Clinical Events (CHALICE) Rule, and the Canadian Assessment of Tomography for Childhood Head injury (CATCH) Rule
PECARN HEAD IMAGING DECISION RULES
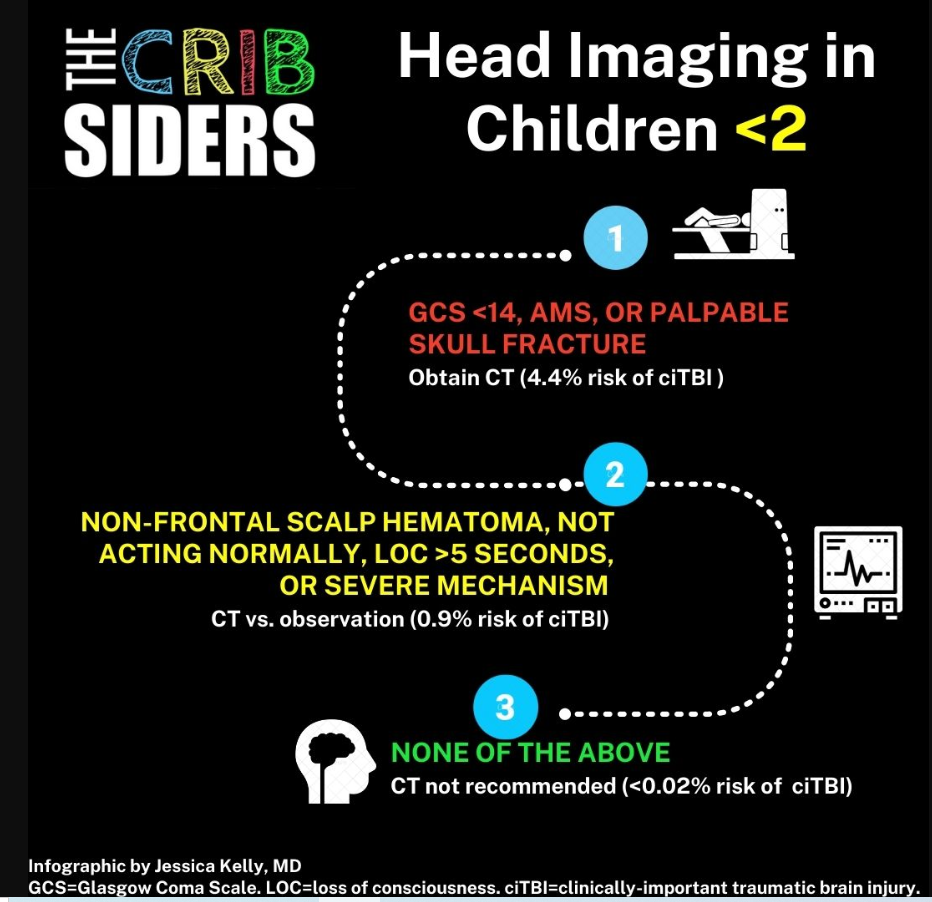
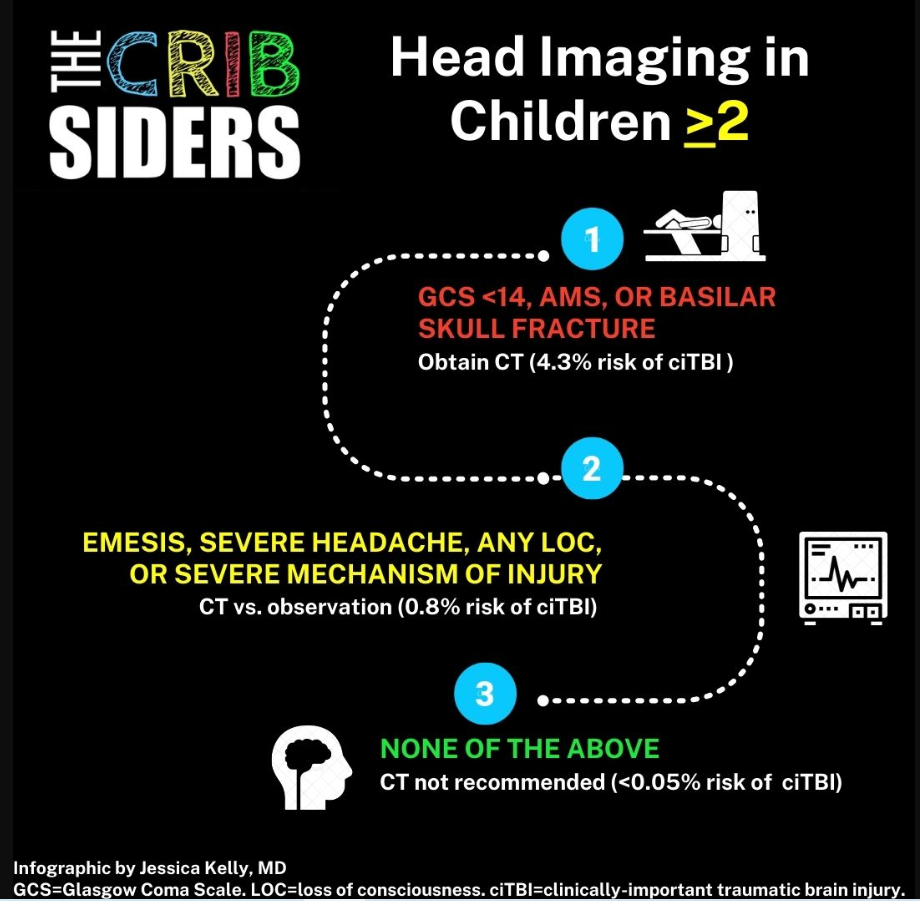
- Looked at over 40,000 kids with minor head injury and developed a CT imaging algorithm for children <2 years and >2years old (Kuppermann et al. Lancet 2009)
- When deciding whether to obtain neuroimaging vs. observe, take into account caregivers’ preferences and ability to closely monitor patients after discharge
- Children with a severe mechanism of injury, such as fall of 3 feet of more (<2 years old) or fall of 5 feet or more (>2 years old), have a greater risk of brain injury and fall into the CT vs. observation category
- Editor’s note: Severe mechanism also includes MVC with patient ejection, death of another passenger, or rollover; pedestrian or bicyclist w/o helmet struck by motorized vehicle; head struck by high-impact object
PECARN RULES FOR CHILDREN <2
- If GCS <14, altered mental status, or palpable skull fracture → Obtain CT (4.4% risk for brain injury)
- If occipital/parietal/temporal scalp hematoma, not acting normally per parent, LOC >5 seconds, or severe mechanism of injury → 0.9% risk for brain injury → CT vs. observation based on clinical experience, multiple findings, worsening symptoms, and parental preference
- If none of the above → CT not recommended
PECARN RULES FOR CHILDREN >2
- If GCS <14, AMS, or basilar skull fracture → Obtain CT (4.3% risk for brain injury)
- Emesis, severe headache, any LOC, or severe mechanism of injury → 0.8% risk for brain injury → CT vs observation based on clinical experience, multiple findings, worsening symptoms, and parental preference
- If none of the above → CT not recommended
ABBREVIATED (ALSO SOMETIMES CALLED FAST OR QUICK) MRI
- MRI is as feasible and accurate as CT imaging to identify TBI (Lindberg et al. Pediatrics. 2019)
- 6 minute brain MRI focused on identifying TBI which details the exact sequences of an MRI protocol available for reproducibility (Lumba-Brown et al. JACEP Open. 2020)
- Pros: MRI avoids the dose of radiation that CT delivers
- Cons: Nondisplaced skull fractures are better diagnosed on CT. However, diagnosing nondisplaced skull fractures often does not change management. MRI can usually diagnose displaced skull fractures.
- MRI and CT can both identify traumatic intracranial hemorrhage
OBSERVATION IN MTBI
- Expert Opinion: Depends on what the patient looks like and can range from 1 hour to several hours. You need to get an initial exam and second exam to understand if the patient is improving, worsening, or staying the same. In the middle of the night, when a child is normally sleepy, you may need to observe longer than you would during the day
- Red flags during observation: worsening of symptoms or headache, change in mental status, increasing agitation, and other signs of late-stage elevated intracranial pressure (e.g., hypertension, bradycardia, and irregular respirations)
- Serial exams are patient-specific. Make sure the patient can engage with you, make eye contact, speak to you, move all of their extremities, and is easily moving their head/neck
Diagnostic adjuncts
- Oculomotor function: can be measured with augmented reality goggles in specialty concussion clinics
- Post-concussion symptom scale: Many scales are available, choose one you like such as the Post-Concussion Symptom Scale (PCSS) or CDC Acute Concussion Evaluation (ACE) Form Complete the form and have the patient track their symptoms at home to see how their symptoms are developing over time
- Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT): Neurocognitive computer-based test that athletes complete, will identify cognitive impairments if present
Concussion subtypes/phenotypes
There are 5 concussion subtypes (Lumba-Brown et al. Neurosurgery. 2020)
- Headache/Migraine
- Oculomotor
- Vestibular
- Anxiety/Mood disruption
- Cognitive
CONCUSSION-ASSOCIATED CONDITIONS
- Cervical strain injury: Can present similar to mTBI in symptomatology
- Sleep Disturbance: Very common
CHRONIC TRAUMATIC ENCEPHALOPATHY (CTE)
- Repeated head injuries can result in CTE
- Must balance the benefits of sports (physical and social) with the risk of head injuries
RECOVERY AND TREATMENT
- Most children recover in 1 month
- 30% of children will have symptoms that persist beyond 1 month (Lumba-Brown et al. JAMA Pediatr. 2018). These children may benefit from additional therapies
- Treatment plans must include strategizing a plan for recovery and securing adequate follow-up and/or subspecialty referrals as needed
- Headache symptoms can be treated with PRN ibuprofen and acetaminophen, sunglasses if light is a trigger, and seeking out quiet places if noise is a trigger. Do not use narcotics
- Oculomotor dysfunction can be treated with oculomotor rehabilitation and eye exercises
- Vestibular impairment can be treated with vestibular rehabilitation
- Neuropsychologists can help with anxiety and mood disruption
- Emphasize sleep hygiene, bright light during the day, staying on a set bedtime, quiet sleep environment, prioritizing sleep, and melatonin PRN
- Deep breathing in concussion can help reduce symptoms (Cook et al. Dev Neurorehabil. 2020)
- Reassure parents, counsel them on what to expect, and validate symptoms
- Referral to a specialist (concussion clinic) depends on a provider’s comfort with mTBI. If patients have a significant symptom burden, symptoms >1 month, or symptoms that are affecting their ability to complete their daily activities, they deserve further evaluation. Concussion clinics have access to advanced diagnostic adjuncts, objective tests of mTBI and access to specific resources for rehabilitation and therapy
RETURN TO ACTIVITY
- Reintegrate into cognitive and physical activities after 2-3 days of rest (Lumba-Brown et al. JAMA Pediatr. 2018)
- Aerobic activity can decrease symptom duration (Lumba-Brown et al. JAMA Pediatr. 2018)
- Engage in activities as tolerated and take breaks when needed
- After a head injury, children are at a lower threshold for re-injury. They should not engage in risky play or contact sports when recovering from a concussion. Players should assume they will be out of contact play for 2-4 weeks
- Communicate with pediatricians and teachers that children may need an individualized learning plan with more time to complete work or reduced workload
HEALTH DISPARITIES IN CONCUSSION
- Sex disparities: Most of the literature about mTBI is based on males who sustained head injuries in sports. Females manifest mTBI differently than males. One recent study found females had a longer recovery time than males (Rosenbaum et al. JAMA Netw Open. 2020)
- It is our responsibility to ask questions about our patients’ home, social environment, school supports, access to follow-up care, and assess for other stressors that may affect recovery
- Patients who were socioeconomically disadvantaged were more likely to have poor outcomes (Zonfrillo et al. J Neurotrauma. 2014)
- Black children are 30% less likely than non-hispanic counterparts to be diagnosed with a sports-related concussion when presenting with head injury (Lyons et al. 2019. Front Neurol)
- Black adolescents were less likely than white adolescents to be diagnosed with concussion when presenting with head injury (Wallace et al. J Emerg Med. 2020)
TAKE HOME POINTS
- Consider mTBI following any head injury
- Consider the 5 subtypes of concussion
- Ask patients about sleep disruption and cervical strain
- Remember that each concussion presents individually
- If you choose not to obtain neuroimaging in the acute setting, ensure you are sending the child home with a reliable caregiver who lives relatively close to the hospital and understands the warning signs to look out for
- Counsel families on what mTBI looks like, what to expect with mTBI, and offer reassurance that most children will recover in one month