Need to review this and put it in post: Antiphosphospholipid syndrome presenting with amaurosis fugax and cotton wool spots.
Emergency Medicine Cases had a great brief talk on Transient Monocular Vision Loss on EM Quick Hits 5 [Link is to the podcast and show notes and here is the direct link to podcast.] June 2019 [9:20 – 16:15] by Dr. Anna MacDonald. As these are my study notes, I’ve included Dr. MacDonald’s lecture notes:
Transient Monocular Vision Loss (TMVL)
Causes of TMVL
- Non-inflammatory vascular causes
- Emboli (TIA of the eye)
- Ocular ischaemia
- Impending Central Retinal Vein Occlusion (CRVO)
- Giant cell arteritis (temporal arteritis)
- Retinal migraine (VL should be followed by headache within 60 mins)
- Optic neuritis – Uhthoff’s phenomenon
- Local globe/orbit/lid problems (e.g.
- glaucoma, orbitopathies, hyphema, dry eyes)
Clinical Pearls
- TMVL from emboli is very difficult to differentiate clinically from GCA. Have a low threshold to do ESR and CRP in patients over 50.
- Much more likely to be arterial ischaemia if:
- Clear description of sudden onset and specific duration of vision loss
- Description of curtain coming down or up over field of vision
What follows are excerpts from Update on the evaluation of transient vision loss [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Clin Ophthalmol. 2016 Feb 11;10:297-303. doi: 10.2147/OPTH.S94971. eCollection 2016.
Introduction
A proper, well-performed history and physical exam after an episode of transient vision loss (TVL) improves the chance of finding its cause. Determining the etiology of TVL will guide management.
TVL is not always interchangeable with “amaurosis fugax”. Most ophthalmologists
use the term amaurosis fugax when they suspect a thromboembolic vascular etiology
as the cause of monocular TVL.1 . . . Because many
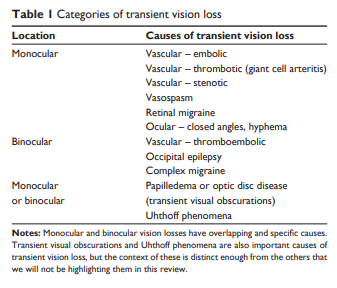
patients present to an ophthalmologist with TVL as the harbinger of cerebrovascular disease,2 it is important to be aware of their future potential for stroke, but not pigeonhole all TVL into amaurosis fugax. Table 1 lists the major causes to consider when a patient presents with TVL.
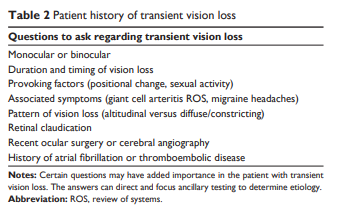
Obtaining a history in patients
with TVLThe pattern of visual field loss* during an episode of TVL provides prognostic information. Patients with altitudinal TVL are more likely to have a carotid or cardiac embolic source compared to patients with diffuse or constricting patterns of vision loss.3 Altitudinal TVL increases the odds of internal carotid artery stenosis by 3.5.4,5 . . . Since ~40% of patients with an altitudinal defect at the start of TVL progress to a diffuse or total vision loss,3 it is important to specifically ask about how the TVL was perceived at its onset. A smaller percentage of patients have a vertical hemifield TVL.3
*See Visual Field Testing: From One Medical Student to Another, by Joy N. Carroll and Chris A. Johnson, Ph.D. Published August 22, 2013 from EyeRounds.org.
In contrast, characteristics of the TVL are less helpful in predicting the nature of future ocular vascular events. No differences in the character of field defects during a TVL differentiate whether a patient will later develop a central retinal artery occlusion (CRAO), retinal vein occlusion, nonarteritic anterior ischemic optic neuropathy, or giant cell arteritis (GCA). There is also no correlation between time lapse from the TVL to when permanent vision loss would occur and the cause of the permanent vision loss.6
Retinal claudication is one historical
feature predicting complete carotid occlusion. Dimming of vision in one eye after exposure to bright light after TVL has an odds ratio of 4.8 for finding 100% ipsilateral carotid occlusion.5
Even if the patient is not able to recall much
history, this “lack” of information itself may be helpful: patients unable to remember details of their TVL are more likely to have normal carotid arteries.5Table 2 summarizes historical information important to obtain in a patient with TVL.
TVL and thromboembolic vascular
diseaseGeneral considerations
Public awareness that TVL could be a transient ischemic attack (TIA) is low: between 7% and 44%.11,12 This compares to 80%–90% of people who recognize that speech, face, and arm symptoms are associated with stroke.13 Compared to other TIA symptoms, patients with TVL arrive less quickly
to the emergency room.14Regarding the incidence of TVL in TIA, one study
examined 2,398 patients with suspected TIA over 5 years. In all, 826 (34.5%) reported transient visual symptoms and 422 (17.6%) had “only” visual symptoms. Of these, 36.3% had TVL, 12.3% transient hemianopia, 10.8% bilateral positive visual phenomena, and 4.5% bilateral total vision loss.17 A study from Japan of 444 patients admitted to a
TIA center reported 2.9% presenting as TVL.14 What is the incidence of carotid disease in patients with TVL? Of 337 patients with transient monocular vision loss studied prospectively, 159 had a normal internal carotid artery patency, 33 had 0%–69% stenosis, 100 had 70%–99% stenosis, and 45 had 100%.5Carotid disease
Resume here.
Note to myself: Review my post on Eval of Stroke and TIA for how to workup TIA.]
Stroke And TIA – Help From MCHD Paramedic Podcast, EMC Podcast, And emedicine.medscape.com
Posted on March 12, 2019 by Tom Wade MD