The following is from p S54 of Resource (2)
Hypoglycemia
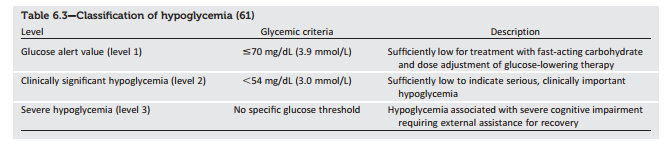
Hypoglycemia is the major limiting factor in the glycemic management of type 1 and type 2 diabetes. Recommendations from the International Hypoglycaemia Study Group regarding the classification of hypoglycemia are outlined in Table 6.3 (61). Of note, this classification scheme considers a blood glucose ,54 mg/dL (3.0 mmol/L) detected by SMBG, CGM (for at least 20 min), or laboratory measurement of plasma glucose as sufficiently low to indicate serious, clinically significant hypoglycemia that should be included in reports of clinical trials of glucose-lowering drugs for the treatment of diabetes (61). However, a glucose alert value of $70 mg/dL (3.9 mmol/L) can be important for therapeutic dose adjustment of glucose-lowering drugs in clinical care and is often related to symptomatic hypoglycemia. Severe hypoglycemia is defined as severe cognitive impairment requiring assistance from another person for recovery (62).
In 2015, the ADA changed its preprandial glycemic target from 70–130 mg/dL (3.9–7.2 mmol/L) to 80–130 mg/dL (4.4–7.2 mmol/L). This change reflects the results of the ADAG study, which demonstrated that higher glycemic targets corresponded to A1C goals (27). An additional goal of raising the lower range of the glycemic target was to limit overtreatment and provide a safety margin in patients titrating glucose-lowering drugs such as insulin to glycemic targets.
Hypoglycemia Treatment
Providers should continue to counsel patients to treat hypoglycemia with fast-acting carbohydrates at the blood glucose alert value of 70 mg/dL (3.9 mmol/L) or less. Hypoglycemia treatment requires ingestion of glucose- or carbohydrate-containing foods. The acute glycemic response correlates better with the glucose content of food than with the carbohydrate content of food. Pure glucose is the preferred treatment, but any form of carbohydrate that contains glucose will raise blood glucose. Added fat may retard and then prolong the acute glycemic response. Ongoing insulin activity or insulin secretagogues may lead to recurrent hypoglycemia unless further food is ingested after recovery. Once the glucose returns to normal, the individual should be counseled to eat a meal or snack to prevent recurrent hypoglycemia.
Glucagon
The use of glucagon is indicated for the treatment of hypoglycemia in people unable or unwilling to consume carbohydrates by mouth. Those in close contact with, or having custodial care of, people with hypoglycemia-prone diabetes (family members, roommates, school personnel, child care providers, correctional institution staff, or coworkers) should be instructed on the use of glucagon kits including where the kit is and when and how to administer glucagon. An individual does not need to be a health care professional to safely administer glucagon. Care should be taken to ensure that glucagon kits are not expired.
Hypoglycemia
Prevention Hypoglycemia prevention is a critical component of diabetes management. SMBG and, for some patients, CGM are essential tools to assess therapy and detect incipient hypoglycemia. Patients should understand situations that increase their risk of hypoglycemia, such as fasting for tests or procedures, delayed meals, during or after intense exercise, and during sleep. Hypoglycemia may increase the risk of harm to self or others, such as with driving. Teaching people with diabetes to balance insulin use and carbohydrate intake and exercise are necessary, but these strategies are not always sufficient for prevention.
In type 1 diabetes and severely insulindeficient type 2 diabetes, hypoglycemia unawareness (or hypoglycemia-associated autonomic failure) can severely compromise stringent diabetes control and quality of life. This syndrome is characterized by deficient counterregulatory hormone release, especially in older adults, and a diminished autonomic response, which both are risk factors for, and caused by, hypoglycemia. A corollary to this “vicious cycle” is that several weeks of avoidance of hypoglycemia has been demonstrated to improve counterregulation and hypoglycemia awareness in many patients (68). Hence, patients with one or more episodes of clinically significant hypoglycemia may benefit from at least shortterm relaxation of glycemic targets.
Resources:
(1) CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2017 EXECUTIVE SUMMARY [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Endocr Pract. 2017 Feb;23(2):207-238. doi: 10.4158/EP161682.CS. Epub 2017 Jan 17.
(2) AMERICAN DIABETES ASSOCIATION STANDARDS OF MEDICAL CARE IN DIABETES—2017 [Full Text PDF]. January 2017 Volume 40, Supplement 1.
(3) Patient-directed titration for achieving glycaemic goals using a once-daily basal insulin analogue: an assessment of two different fasting plasma glucose targets – the TITRATETM study [PubMed Abstract] [Full Text HTML] [Full Text PDF]. Diabetes Obes Metab. 2009 Jun;11(6):623-31. doi: 10.1111/j.1463-1326.2009.01060.x.