Soon, I’ll be taking the Pediatric Advanced Life Support Recertification Course and so I’m starting my PALS review. This post is part of that review.
For patients less than 8 years old, experts recommend percutaneous needle tracheostomy when a surgical airway is needed.
After reviewing pediatric anesthesiologist Dr. Fiadjoe’s CHOP lecture Airway Management: Lessons Learned From The PEDI [Pediatric Difficult Intubation] Multicenter Registry, I was motivated to revisit pediatric needle cricothyrotomy. The point of his excellent lecture was that pediatric airway management can be hard even for pediatric anesthesiologists. And for peds patients weighing less than 10 kg, airway management is even harder.
One thing Dr. Fiadjoe recommends is that if your first attempt fails, try something different because anything more than 2 attempts causes a markedly increased rate of complications.
So maybe your first attempt is with direct or video laryngoscopy. And if you fail on your first attempt you need to do something different, maybe direct if you used video first, or vice versa. Or maybe your second attempt could be with an laryngeal mask airway of some sort. So be sure to review Dr. Fiadjoe’s outstanding CHOP lecture.
So in addition to the YouTube video below, I’ve included links in Resources below to two additional resources:
- Pediatric Needle Cricothyrotomy: A Case for Simulation in Prehospital Medicine from MedEdPORTAL – The Journal of Teaching and Learning from the Association of American Medical Colleges.The article contains links to ten appendices that you must download and review. The content is in the appendices.
- Neonatal Resuscitation Program: Use of the Laryngeal Mask Airway
Posted on September 22, 2014 by Tom Wade MD
Here is the excellent YouTube video. I have included some screen shots below.
Here are some screen shots with accompanying narrative:
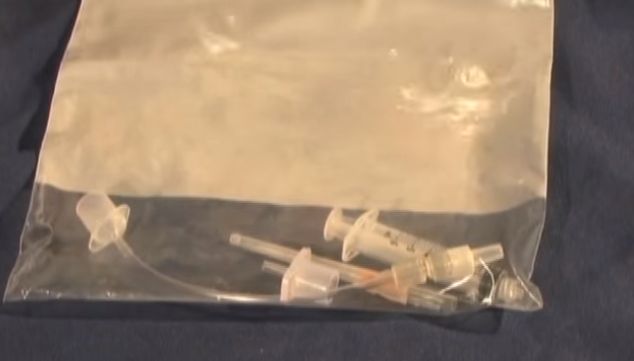
Screen Shot 1:
Screen Shot 2:
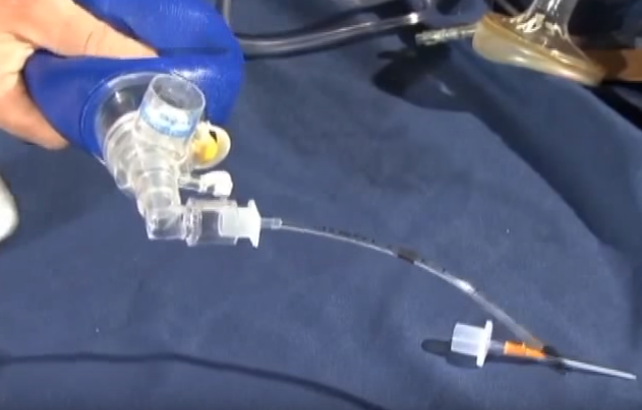
This is the preassembled kit for percutaneous needle tracheostomy or PNT.
It should be made up in advance to make sure the components fit together.
The kit should be kept in an accessible place in the emergency department.
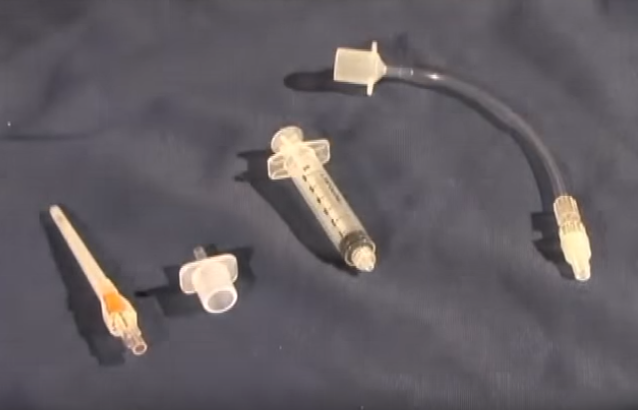
Screen Shot 3:
These are the components:
- a 14 gauge catheter
- the adapter from a 3.5 ET tube
- a 5 cc syringe
- and an extension set made up of six inches of IV tubing with a luer lock attatched to a 2.5 ET tube adapter.
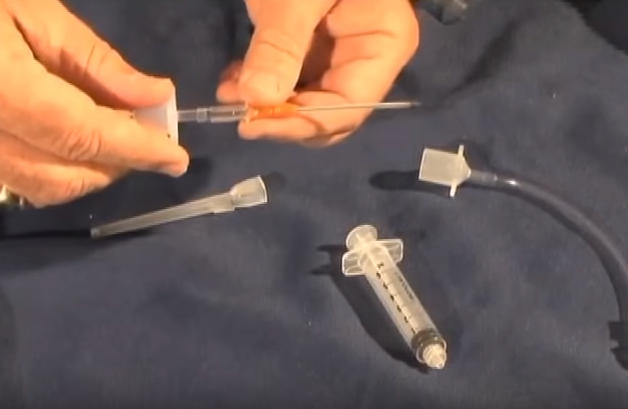
Screen Shot 4:
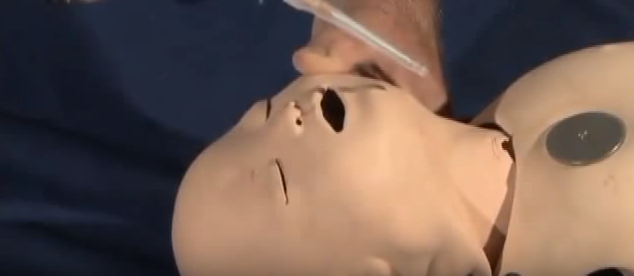
Once the catheter has been inserted into the trachea, and the needle removed, it can be attached to the 3.5 ET tube adaptor.
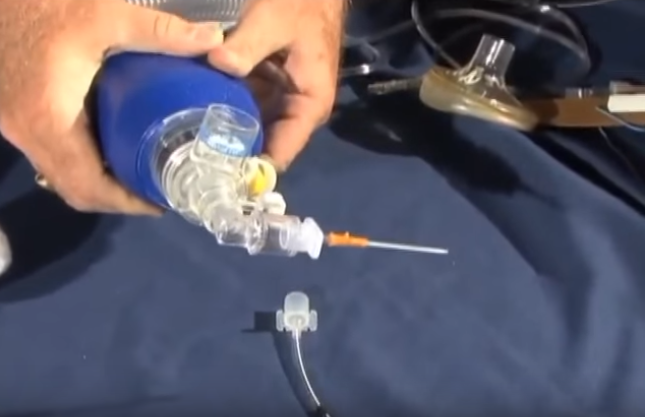
Screen Shot 5:
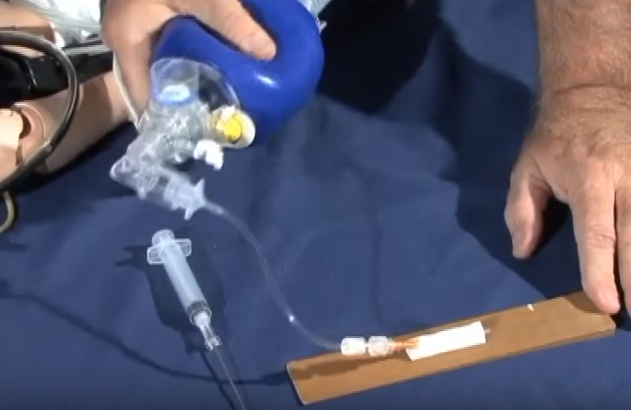
The popoff valve on the bag-valve-mask needs to be closed because bagging through a lumen as narrow as the catheter creates resistance to flow requiring pressures greater than 40 cm of water to optimize flow.
Screen Shot 6:
Compare this resistance [through the 14 gauge catheter] with that of ventilating through a 3.5 mm ET tube. You need to connect the catheter to feel the amount of resistance produced so that you will not doubt your catheter placement should you ever have to do this procedure yourself.
Screen Shot 7:
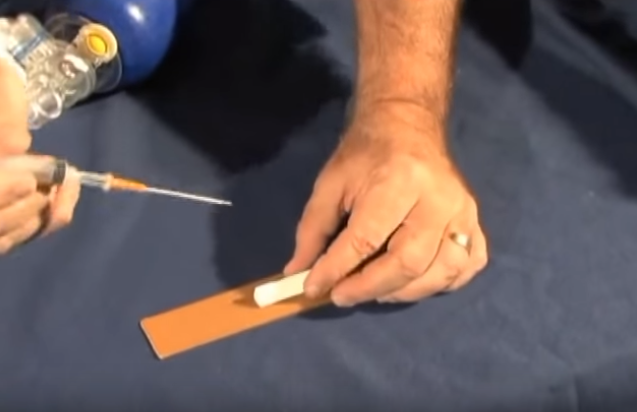
When inserting the catheter into the trachea, enter at the shallowest angle possible.
Some clinicians prefer to use a syringe filled with saline attached to the catheter so an air bubble will be seen when the catheter enters the trachea and air escapes. . .
Screen Shot 8:
. . . much like the return of blood when starting an IV as an aid to successful placement.
Screen Shot 9:
One of the complications in animal studies of this procedure was kinking or obstruction or obstruction of the catheter when directly attatched to a bag-valve-mask. This can be avoided by interposing an extension set made up of six inches of IV tubing with a luer lock [at the end of the IV tubing attached to the 14 gauge catheter] attached to a 2.5 ET tube adapter. This will allow more freedom of movement for the bag-valve-mask without the danger of kinking the catheter.
Starting at 2:41 in the video, the speaker discusses other alternatives including a commercial device from Cook, the ENK Oxygen Flow Modulator, which has been discontinued.
And next the speaker strongly warns against using the Jet Ventilator.
We do not recommend using the it [the Jet Ventilator] for ventilation in children. The excessively high pressures are not needed and the flow rates produced by this apparatus are extremely dangerous, easily causing barotrauma.