Today, I reviewed, excerpt from and link to Evaluation Of The Limping Child [PubMed Abstract] [Download the PDF]. Jessica Burns, MD, MPH; Scott Mubarak, MD
Rady Children’s Hospital, San Diego, CA. JPOSNA® (the Journal of the Pediatric Orthopaedic Society of North America) is an open access journal focusing on pediatric orthopaedic conditions, treatment, and technology. 2020.
All that follows is from the above resource.
Abstract: Prompt evaluation of a younger child (age <5) with gait disturbance or refusal to walk is necessary to
distinguish orthopedic urgency (trauma or infection) from relatively benign processes and chronic problems such as
arthritis. Physical examination should include evaluation of gait, supine and simulated prone hip examination (on the
parent’s lap to keep the child comfortable), and the crawl test. There are six radiographic views of the lower
extremities that can assist in the diagnosis. In conjunction with the detailed history, a thorough physical exam, and
radiographs from the orthopedic provider can determine the need for laboratory tests and other imaging.Key Concepts:
• Evaluation of the limping child begins with a thorough history.
• Physical examination of the limping child can be optimized by utilizing the parent to hold the child while the examiner moves the extremities and checks the back.
• Six screening radiographs can be obtained to assist in making the correct diagnosis.
• Laboratory analysis and magnetic resonance imaging can be obtained if the diagnosis remains elusive.Onset: Acute trauma is more likely if there was a fall
and the child cried and failed to walk immediately
thereafter. If there was a delay in the onset of the limp
or pain; or history of trauma is unclear, infection or
synovitis is more likely. Additionally, the duration of
the symptoms should be appreciated in the context of the
trajectory of those symptoms. Worsening of symptoms
would add support for an infectious/inflammatory
process rather than trauma.To help determine trauma from inflammatory causes, the examiner should ask the following questions:
• Was the injury witnessed?
• Did the child cry immediately after the fall?
• When did the child start to limp—immediately?
• If the child won’t walk, will he or she crawl?
• Are there any puncture wounds?Position: The caretaker should be asked regarding the
side involved, and if the child is limping or unable to
bear weight completely. If the child is not walking, the
examiner should inquire regarding the ability of the child
to crawl. A normally ambulatory child who can crawl
has the ability to bear weight through the femur and hip
and knee, and the inability to walk is likely due to
pathology in the tibia or foot.Quality/severity: Characterization of the pain in terms of
being constant or intermittent can be beneficial. Constant
pain is more indicative of an interosseous process such
as infection or developing tumor. When there is a clear
fracture and no history of trauma given, pathological
fracture or child abuse should be considered.1,8Timing: The time of day that the pain occurs should be
obtained. Pain that wakes the child from sleep at night
suggests a more aggressive process rather than pain after
intense activity. Morning pain associated with stiffness of the joints suggests an inflammatory process, including
rheumatologic conditions.8,9A limp is any deviation of the normal gait cycle that can
appear irregular, asymmetric, laborious, or erratic. The
etiology of an abnormal gait can result from pain,
weakness, mechanical alterations, or neurologic
abnormalities. An antalgic gait is characterized by
decreased duration of stance on the affected side,
decreasing the time spent bearing weight can reduce
pain. This also reduces the stride length of the opposite
limb.6
Antalgia can present with a guarded gait that can
appear like a slow, shuffling gait, as the presentation can
occur with spine related pathology.*7
*For example, discitis.
Discitis is an uncommon condition that causes swelling and irritation of the space between the bones of the spine1. It is usually seen in children younger than 10 years and in adults around 50 years of age, and men are more affected than women1. Diskitis can be caused by an infection from bacteria or a virus1. Diagnosis is made with blood cultures and MRI studies2. Treatment is bed rest, immobilization, and antibiotics for 4-6 weeks for early infection with no abscess2.Learn more:
Physical Exam (see video)*Gait observation should be done where there is plenty of
space and the ability for the child to move without
changing the gait due to obstacles. The gait can be
observed prior to the formal history and physical, if the
examiner is able to see the child mobilize down the
clinic hallway or in the emergency department.8,10
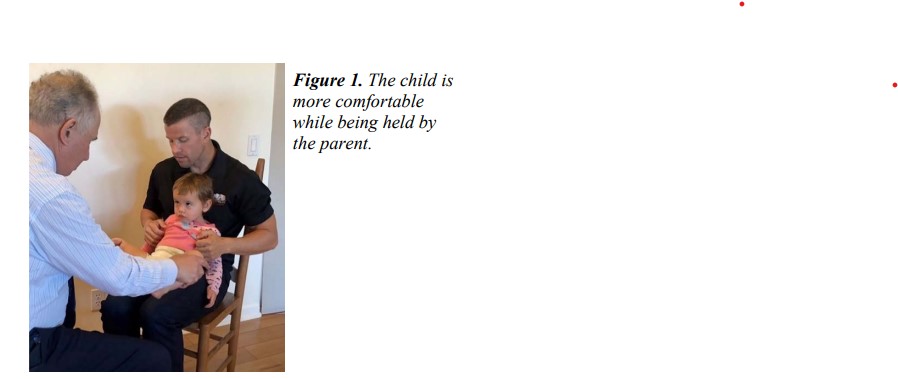
The physical examination of the child should utilize the
parent in promoting gait and providing comfort while
moving through palpation and passive range of motion
of the back and lower extremities. This portion of the
exam should be done gently and quietly on the parent’s
lap (Figure 1). In order to grain trust, the examination
should start with areas that are clearly not the source of
pathology. Palpate the back, pelvis, and trochanters, then
move distally and palpate the distal femurs, tibias and
feet. Look for knee and ankle swelling. Once the child
is comfortable in the parent’s lap, the examiner should
finally attempt to localize the area of pain. Always save
the portion of the exam that might be painful for last and
avoid any noxious tests such as blood draw for the end.
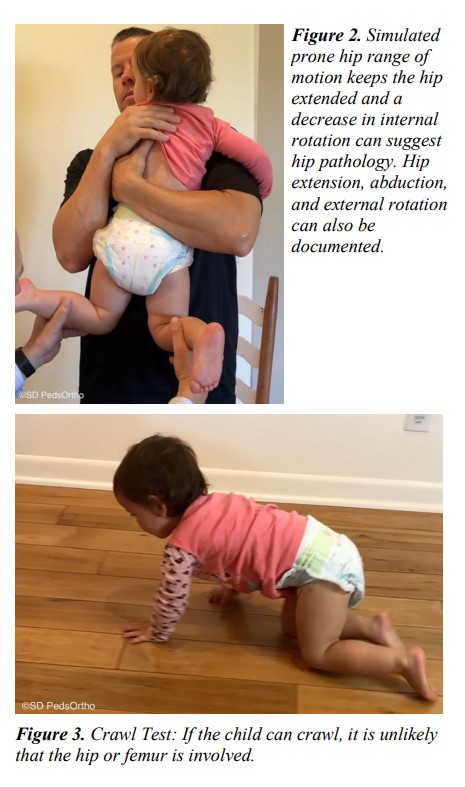
Two helpful tests are:1. Simulated prone internal rotation of the hip
(Figure 2): For the younger child, this is best done with
the child held by the parent chest to chest, with hips fully
extended. The extended position increases joint pressure
by decreasing the volume of the joint capsule.Furthermore, this position provides a more accurate
measure of the hip’s internal rotation compared to the
normal side by stabilizing the child’s pelvis. This is the
most sensitive indicator of hip joint involvement for
subacute disorders ranging from synovitis, arthritis, and
Perthes disease. Even hip flexion, extension, and
abduction can be done from this position.
2. Crawl Test (Figure 3): This will be most useful for
lateralization and localization of the pathology. If the
child will not stand, try to entice the child to crawl. If by history or by exam a reciprocal crawl is possible, the
pathology is distal to the knee. Pelvis osteomyelitis and
hip and knee sepsis are extremely unlikely in the child
who can crawl, and physical examination and imaging
studies can now be limited to the leg and feet. Examples
of pathology that limits crawling include tibia fracture,
osteomyelitis of the distal tibia, foot fracture,
osteochondritis of the foot (Kohler disease, etc.), or
foreign body in the foot.
RadiographsStart here