Today, I link to and excerpt from the Curbsiders‘ #101:Cirrhosis: Medications, decompensation, complications
JUNE 25, 2018 By CYRUS ASKIN [Link is to the show notes and pocast]
All that follows is from the above resource
Cirrhosis. Take control of cirrhosis and treat your patients like the pros! In this episode of The Curbsiders, Dr. Scott Matherly, assistant professor in the Dept of Medicine at Virginia Commonwealth University and board certified hepatologist, builds upon his introduction to cirrhosis. You already know what to look out for and how to diagnose these patients, now it’s time to build your knowledge and medical repertoire against this deadly condition! Topics include: high protein diet, ascites, diuretics, hepatic encephalopathy, lactulose vs rifaximin, portal hypertension, esophageal varices, beta blockers, spontaneous bacterial peritonitis prophylaxis and more pathophysiology!
Goal: In contrast to Dr. Matherly’s first episode which focused on introducing cirrhosis, this episode will equip listeners with the tools to manage cirrhosis like a pro! You will learn about the pathophysiology of cirrhosis and the “separate but connected” problems that every cirrhotic will face. Most importantly, in this episode Dr. Matherly take us on a tour of the medications that comprise our armamentarium against cirrhosis and describes when they are best used.
Clinical Pearls
- In NASH interventions such as Vitamin E, Pioglitazone and Liraglutide all seem to have some evidence suggesting they may help prevent or even reverse cirrhosis (PIVENS Trial, Pioglitazone in NASH, LEAN Trial ).
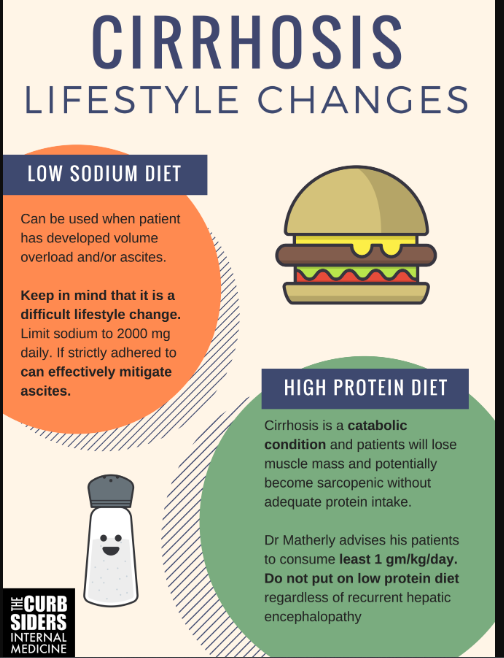
- Lifestyle modifications, such as high protein diets and sodium restriction (under 2000 mg daily) can be useful in managing cirrhotic patients when utilized appropriately.
- The cirrhotic condition is characterized by parenchymal liver disease and portal hypertension. It is generally the sequelae of portal hypertension to which most therapies are targeted. -Dr Matherly
- Treatment of ascites: Spironolactone can be used as monotherapy (PMID 12873814) or in combination with furosemide in ratio of 100 mg spironolactone to 40 mg furosemide. Furosemide monotherapy is more likely to cause hypokalemia (PMID 7035545)
- Hepatic encephalopathy (HE): Most feared complication by patients due to unpredictability and amnestic effects. Tell patients to self titrate lactulose to three bowel movements daily. Mechanism of action remains controversial. -Dr Matherly
- Treatment of HE: Lactulose and/or rifaximin for hepatic encephalopathy, non-selective beta-blockers for varices, and medications like midodrine, and octreotide for hepatorenal syndrome.
- Dr. Matherly: Spontaneous bacterial peritonitis (SBP) antibiotic prophylaxis is not for everyone.
- Secondary prophylaxis is strongly recommended. -Dr Matherly
- Cautiously consider primary prophylaxis in patients with risk-factors for infection, especially in the era of C. difficile and antibiotic resistance -Dr Matherly
- Mortality: In the decompensated cirrhotic with ascites, around 45% of all-comers will live 5 years from the time of decompensation. (PMID 24128415)
What may delay the progression of NASH to cirrhosis?
- Vitamin E – PIVENS trial showed evidence of reversing NASH on biopsy, but this trial excluded diabetics and cirrhotics! PIVENS Trial (Wiki JC Link)
- Pioglitazone – Recent evidence shows it may work (Bril F et al. Clin Gastroenterol Hepatol. 2018), but watch out for side effects: weight gain, osteoporosis, water retention.
- Liraglutide – Some evidence for histologic resolution of NASH (LEAN Trial)
What lifestyle modifications can be considered at the time of diagnosing cirrhosis?
Low sodium diet
- Useful in patients with ascites or hypertension
- Difficult to maintain because food tastes bland. Only recommend if absolutely necessary. -Dr Matherly
- However, a low sodium diet that is strictly adhered to may be enough to mitigate ascites in some patients
High protein diet
- May be helpful given the catabolic nature of cirrhosis
- At least 1 gm/kg/day -Dr Matherly
- Do not put on low protein diet regardless of recurrent hepatic encephalopathy
Think of Cirrhosis as a disease process with “two separate but connected problems” – Dr. Matherly
- Hepatic Parenchymal Disease – High MELD, elevated bilirubin, INR and eventually hepatocellular carcinoma. Impaired synthetic function (protein, clotting factors, etc.)
- Portal Hypertension: elevated blood pressure in the portal vein which drains the gut
Pathophysiology and complications
- Ascites – Increased pressure in hepatic sinusoids (capillaries of liver) leads to increased fluid/hydrostatic pressure and decreased oncotic pressure (low albumin) leads to fluid spilling out into liver parenchyma which then weeps into the peritoneal cavity.
- Hepatic encephalopathy (HE) – a clinical diagnosis with signs including: slow to answer questions, repetitive speech, reversal of sleep-wake cycle
- Ammonia levels are generally not useful because they do not correlate with levels of hepatic encephalopathy, but consider checking ammonia in the encephalopathic patient without known liver disease or as a prognostic tool in the patient with acute liver failure.
- Varices – the portal vein drains entire gut from the lower third of the esophagus to the rectum; portal hypertension causes gastric and esophageal varices
- Circulatory dysfunction with hypotension – a hallmark of cirrhosis
- Cirrhosis and portal hypertension, complicated by inappropriate levels of nitric oxide, results in pooling of blood in splanchnic (gut) circulation
- This in turn causes relative systemic hypoperfusion
- Leads to “high output state” = increased cardiac output
- Release of antidiuretic hormone, renin, angiotensin, aldosterone lead to increased sodium/water avidity leading to further overload of the splanchnic circulation
- Net effects include hyponatremia and systemic hypotension with hepatorenal syndrome as the end-state when the kidney’s “strangle themselves” off from their own blood supply -Dr Matherly
Therapeutic Interventions
Ascites
- Low sodium diet, 2000 mg daily limit (Phillip SG et al. NEJM 2016. PMID: 27557303)
- Diuretics: Loop diuretics and potassium-sparing diuretics are usually dosed together, but spironolactone alone may be just as effective (Santos J et al. J Hepatol. 2003 PMID: 12873814)
- Dr. Matherly recommends: Step 1 = 40 mg furosemide + 100 mg of spironolactone daily because this ratio seems to maintain normokalemia. This dosing seems to be dogmatic, but effective based on this 1981 study (Fogel MR et al. J Clin Gastroenterol. 1981 PMID: 7035545 PMID ) so we keep doing it!
- Doses can be advanced in increments that maintain 40:100 mg ratio as needed to counteract the kidneys’ sodium avidity and maintain potassium homeostasis.
- Spironolactone: sexual side effects and gynecomastia are a big deal in men, may consider alternative agents (such as eplerenone, but cost is an issue)
Hepatic Encephalopathy – start therapy at the first signs of HE
- Lactulose: first line; nonabsorbable disaccharide
- Don’t really know how this works, but it does!
- Dr. Matherly: Take this medication, change the dose whenever you need to, to have 3 bowel movements daily
- Side effects: bloating, nausea, abdominal discomfort
- Rifaximin: second line
- In patients who need more than lactulose
- Shown to decrease episodes of hepatic encephalopathy (Bass NM et al. NEJM 2010)
- May decrease infections, and mortality
- 550 mg twice daily is well tolerated but very expensive
Varices and Beta-Blockers
- Beta blockers (BB) seem to be beneficial in cirrhotic patients, to a point when used for variceal prophylaxis in patients with large varices or prior variceal bleed. Must use non-selective BB because beta-1 activity reduces cardiac output while the beta-2 activity will lead to unopposed alpha activity and resultant vasoconstriction of the splanchnic vasculature to reduce portal inflow / pressure.
- Discontinue BB in acute kidney injury, systolic BP under 90 mmHg, Na under 120 meq/L (Dr. Matherly / Baveno VI)
Hypotension:
- Goal cited: MAP > 82 (Llach J et al. Gastroenterol. 1988), but practically speaking, it’s difficult to achieve
- Midodrine & Octreotide are reserved for type 1 hepatorenal syndrome
- Midodrine monotherapy: Can use to temporarily increase blood pressure / renal perfusion in ascitic patients who are refractory to diuretics, but this is controversial / not a standard use. -Dr Matherly’s expert opinion
Who needs prophylaxis for Spontaneous Bacterial Peritonitis (SBP)?
- A patient with history of SBP must be on prophylaxis
- In a patient who has never had SBP be much more selective regarding primary prophylaxis. Usually for low-protein ascites + kidney disease or hospitalized / at risk for infection. – Dr. Matherly