As always, I only make excerpts because it helps reinforce my learning. Readers should go to the EMC podcast and post.
Here are additional resources related to Ep 160 to be reviewed:
- Part 1, Ep 159 Geriatric Trauma Part 1: The Under-Triaging Problem, Resuscitation, Airway, Head and C-spine Imaging, Clearing the C-spine.
- Pelvic Fracture Imaging.
Updated: Jul 22, 2021, from emedicine.medscape.com - Assessing Clinical Frailty – Help From Anesthesiology News
Posted on December 10, 2019 by Tom Wade MD - Assessing Clinical Frailty – Help From Anesthesiology News
Posted on December 10, 2019 by Tom Wade MD - The Diagnosis Of Frailty And Its Implications
Posted on March 6, 2018 by Tom Wade MD
In this post I link to and excerpt from Emergency Medicine Cases‘ Ep 160 Geriatric Trauma 2 Rib Fractures, Pelvic Fractures, Prognostication, Elder Abuse, Discharge Planning.*
*Helman, A. Wong, C. Haas, B. Tillmann, B. Geriatric Trauma Part 2: Rib Fractures, Pelvic Fractures, Prognostication, Elder Abuse, Discharge Planning. Emergency Medicine Cases. September, 2021. https://emergencymedicinecases.com/geriatric-trauma-rib-fractures-pelvic-fractures-prognostication-elder-abuse-discharge-planning. Accessed 9-12-2021.
All that follows is from the above outstanding podcast and show notes.
In part 1*of this 2-part podcast series on Geriatric Trauma Barbara Haas, Bourke Tillmann, Camilla Wong and Anton discussed the problem of under-triaging geriatric trauma patients, resuscitation and airway considerations, common injury patterns in the geriatric trauma patient, lab work, head and c-spine imaging, clearing the c-spine in geriatric trauma patients and resuming anticoagulation after minor head injury in the geriatric trauma patient.
* Be sure to review Part 1, Ep 159 Geriatric Trauma Part 1: The Under-Triaging Problem, Resuscitation, Airway, Head and C-spine Imaging, Clearing the C-spine.
In this Episode 160 – Geriatric Trauma Part 2 we answer questions such as: what are the indications for transfer to a trauma center in older patients with rib fractures and why? Can we accurately prognosticate older trauma patients in the ED? How can we best engage family members in goals of care discussions for the older trauma patient? What are the risk factors for elder abuse that we need to be aware of in the ED? How can we best minimize the risk for recurrent falls and bounce backs for the older trauma patient who is discharged from the ED? and many more…
Take home points for geriatric trauma part 2
- Rib fractures are associated with significant mobility and mortality in older adults, especially those with multiple rib fractures – consider transferring these patients to a trauma center
- Treat rib fractures with early multimodal analgesia and/or regional anesthesia; assess pain regularly and mobilize these patients early
- Older adults with hip fractures should ideally be in the OR in <6 hrs to minimize their risk delirium and infection
- Older trauma patients are more likely to break their pelvis, have a lateral compression fracture pattern and to have occult retroperitoneal hemorrhage; bind their pelvis early and get them to angio as soon as they are stabilized
- Older adults with cognitive decline are especially at risk for physical and emotional abuse – if the story doesn’t fit or there are unusual injury patterns, think elder abuse
- When it comes to risk factors for long term morbidity and mortality, the older person’s pre-trauma frailty is perhaps the most important factor to consider, ahead of age and co-morbidities; however prognostication of the older trauma patient is difficult early on – treat patients with the benefit of life in the ED
- For older patients going home after a fall, early mobility is key
- Other discharge planning after a fall should include OT for home safety assessment, falls prevention program, and to connect with the primary care physician to screen for osteoporosis
Rib fractures in geriatric trauma: A significant cause of morbidity and mortality
Rib fractures in geriatric trauma: A significant cause of morbidity and mortality
Isolated rib fractures in younger patients are rarely considered serious injuries and rarely require any specific treatment besides appropriate analgesia. However, age is one of the strongest predictors of mortality after rib fractures, and mortality increases proportionally with each additional rib fracture. Rib fractures are also a surrogate marker for polytrauma, where 90% of patients with multiple rib fractures have additional traumatic injuries. It is therefore important to have a low threshold to image the ribs and chest of older patients after a fall. While CXR with rib views is specific for displaced rib fractures, plain radiographs may miss up to 50% of rib fractures and there is a higher incidence of pulmonary contusions in older trauma patients, so CT is considered the investigation of choice. Additionally, there is a higher incidence of abdominal solid organ injuries in older patients with rib fractures, so consideration should be given to abdominal CT in these patients as well.
Complications of rib fractures in older patients
- 34% go on to develop pneumonia
- Respiratory failure requiring mechanical ventilation
- Pain leading to agitation and delirium
Consider transfer to a lead trauma center if:
- >3 rib fractures or
- Bilateral rib fractures or
- Flail segment (>3 contiguous ribs # in >2 or more place) or
- Any number of rib fractures with significant underlying pulmonary disease
Key goals in ED rib fracture management in older trauma patients
Early pain control with multimodal analgesia, access to regional analgesia, and regular pain assessments. This should include assessing pain at rest (static) and pain on deep breathing/coughing (dynamic). Goals of analgesia include cough with out significant pain and the ability to sit up and roll over independently. If not able to do so, patients are not adequately treated for their pain.
Early mobilization and physiotherapy. This involves clearing the spines as quickly as possible (see Part 1)
Suggested step-wise treatment of rib fracture pain in the geriatric trauma patients 1. Tylenol 650mg PO q6h 2. Ibuprofen 400mg q6h *age, mildly elevated Cr are not absolute contraindications for short term use in the ED 3. Morphine 0.05 mg/kg IV q4h 4. Ketamine 0.1-0.5mg/kg/hr (start at 0.2mg/kg/hr) Regional anesthesia: epidural, serrates anterior, paravertebral blocks etc. (have been shown to reduce mortality and delirium) and may obviate the need for analgesic medications Pitfall: A common pitfall is undertreating pain in older patients with rib fractures in the ED. Treat rib fractures in the older patient with aggressive early multimodal analgesia, regular pain assessment and early ambulation.
Hip and pelvic fractures in geriatric trauma
Hip Fractures and urgency for the OR
Observational studies suggest that delays to operative fixation of hip fractures are associated with higher 30 day mortality, and increased morbidity including pulmonary embolisms, MI and pneumonia.
The HIP ATTACK RCT (2020) – accelerated care defined as time to OR < 6hrs vs. usual care, showed a lower rate of delirium (OR 0.72) and decreased rates of stroke, infection and UTI. However, there were no differences in mortality.
The sensitivity of x-rays for hip fracture is 90–98%. Consider CT in patients with a clinical suspicion for hip fracture with normal appearing hip x-rays.
As in rib fracture ED management it is prudent to employ early analgesia and/or regional anesthesia such as femoral nerve block/fascia iliaca block.
Hip and pelvic fractures in geriatric trauma
Hip Fractures and urgency for the OR
Observational studies suggest that delays to operative fixation of hip fractures are associated with higher 30 day mortality, and increased morbidity including pulmonary embolisms, MI and pneumonia.
The HIP ATTACK RCT (2020) – accelerated care defined as time to OR < 6hrs vs. usual care, showed a lower rate of delirium (OR 0.72) and decreased rates of stroke, infection and UTI. However, there were no differences in mortality.
The sensitivity of x-rays for hip fracture is 90–98%. Consider CT in patients with a clinical suspicion for hip fracture with normal appearing hip x-rays.
As in rib fracture ED management it is prudent to employ early analgesia and/or regional anesthesia such as femoral nerve block/fascia iliaca block.
Pelvic Fractures in the older trauma patient
Older trauma patients are more likely to sustain lateral compression fractures of the pelvis associated with pelvic bleeding requiring transfusion and angiography. It is therefore prudent to consider binding the pelvis early in the resuscitation of the older polytrauma patient with overt or suspected occult hemorrhagic shock. The retroperitoneum is an occult source of bleeding that is generally missed on PoCUS FAST exam. CT with contrast should be considered to evaluate for hemorrhage, especially in the older patient taking anticoagulants. If the initial pelvic x-ray does not reveal an obvious fracture and the patient continues to convey signifiant pain and/or difficulty ambulating, consider CT. Again, early multimodal analgesia is critical in preventing agitation and delirium in these patients.
Pitfall: A common pitfall is to assume that an older patient with a normal appearing hip/pelivs x-ray does not have a fracture; obtain further imaging (eg. CT) in patients who have significant pain or difficulty ambulating in the setting of a non-diagnostic radiograph.
For information on pelvic fracture imaging, please see Pelvic Fracture Imaging.
Updated: Jul 22, 2021 from emedicine.medscape.com
Prognostication and goals of care in older trauma patients
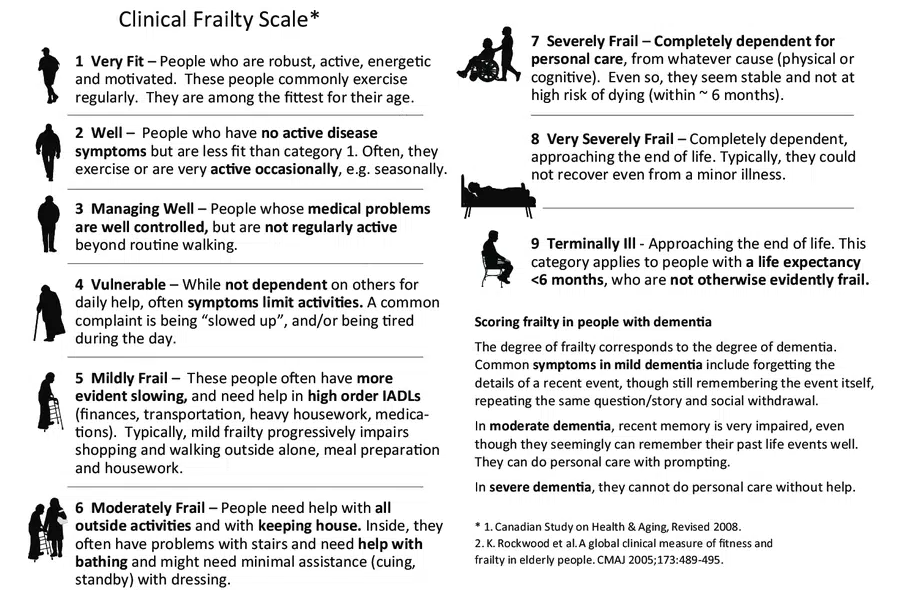
Pre-trauma level frailty (more so than age and co-morbidities) has been associated with poor outcomes. Our experts recommend screening for frailty in all geriatric trauma patients, and there are multiple tools available to do so: (e.g. clinical frailty scale or other validated score).
*For more resources on the diagnosis of and implications of frailty, please see:
- Assessing Clinical Frailty – Help From Anesthesiology News
Posted on December 10, 2019 by Tom Wade MD - The Diagnosis Of Frailty And Its Implications
Posted on March 6, 2018 by Tom Wade MD
The Geriatric Trauma Outcome (GTO) score has also been proposed to estimate the probability of mortality in patients over the age of 65 cared for at a lead trauma center.
GTO Score = age + (2.5 x Injury Severity Score) + 22 (if given pRBC)
Selected GTO scores and their related mortality rate: 205=75%, 233=90%, 252=95%, 310=99%
However, the GTO score could not accurately predict the 1-year mortality. It has been suggested that a frailty score combined with the GTO score to improve prediction of long-term outcomes, but this has yet to be studied.
The IMPACT Score can be used to predict mortality and unfavorable outcomes after TBI. https://www.mdcalc.com/impact-score-outcomes-head-injury
However, even in a frail patient, it is very difficult to provide accurate prognostication in the early course of an elderly patient’s trauma presentation. It is prudent to treat patients with the benefit of life in the ED and engage patients and family members early to establish goals of care.
Bottom line: While frailty, age and co-morbidities are risk factors for poor outcomes after trauma, there is no tool or score that can accurately prognosticate the older trauma patient in the first few hours in the ED. Treat every patient with the benefit of life and engage patients and family soon after your initial trauma resuscitation.
Expert tips on how to engage with families of geriatric trauma patients in goals of care discussions
Establish rapport: “I don’t want to take away any hope, we’re going to do everything we can for your family member.”
Address ageism: “age is just a number – just because they are 85 years old, doesn’t mean we’re going to give up.”
Emphasize honesty and truth, and prepare the family for realistic possible outcomes upfront: “the truth is they have serious injuries and may die from their injuries”
Use specific lay persons language such as “life support” and “life-threatening injuries”
Consider elder abuse in all geriatric trauma patients
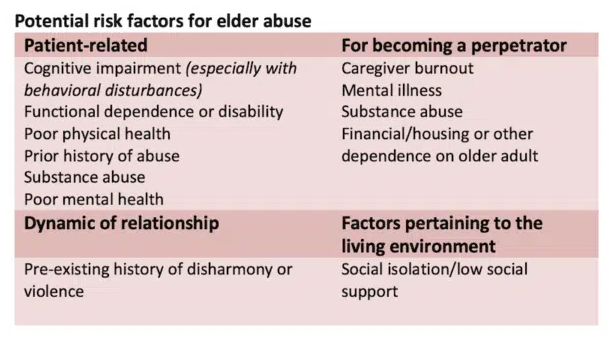
The presence of elder abuse in Canada is reportedly up to 7.5%, with 2-3% in the form of non-accidental trauma. Maintain a high index of suspicion for elder abuse, especially in the elderly trauma patient presenting with unusual injury patterns and inconsistent history. When evaluating older adult trauma patients for abuse, consider established factors that increase the risk for elder abuse.
Identify high risk patients for elder abuse and involve interdisciplinary teams to help address the complex social dynamic involved in elder abuse. Include social work, geriatrics, and other members of the interdisciplinary team to decrease caregiver burden, access adult day program and respite programs, and support for legal action.
Best Practices Guidelines for Trauma Center Recognition of Child Abuse, and Intimate Partner Violence [PDF] from the ACS Trauma Quality Programs.
Discharge planning for the older patient after a ground-level fall
Establish risk for future falls
A person with a single non-injurious fall who has a normal gait and balance is considered at low risk for recurrent falls. Simple tests for gait in the ED include the ‘Timed up and go test’ or ’30 second sit to stand.’
Intrinsic factors: medical illness (Parkinson’s, stroke, diabetes etc.), impaired vision and hearing, age related changes in musculature, gait, and postural reflexes
Extrinsic factors: medications (sedatives & hypnotics, antihypertensives, diuretics, hypoglycemics), improper/lack of assistive devices for ambulation, environmental hazards (lightning, uneven ground, furniture, household clutter)Anyone with any of the below features should be considered at higher risk for falls and should have a multifactorial assessment and intervention plan:
- Presents with a fall resulting in injury
- Gait or balance disorder
- 2 or more falls in the last 12 months
- Frail (e.g. Clinical Frailty Scale 4-9)
Based on the best available evidence to reduce future falls, the discharge plan should also include:
- Referral for an occupational therapy home safety assessment
- Referral to a falls prevention program (gait and balance training and tai chi are some RCT level exercise programs)
- Communication with primary care physician to conduct a falls risk assessment and screen for conditions predisposing to injurious falls (such as osteoporosis)