In this post I link to and excerpt from Dr. Josh Farkas’ Internet Book Of Critical Care [Link is to the Table of Contents] chapter, Hyperthermia & Heat Stroke, January 26, 2017.
All that follows is from Dr. Farkas’ above chapter.
CONTENTS
- Definition & diagnosis of hyperthermia
- Differential diagnosis
- Evaluation
- Treatment
- Algorithm
- Podcast
- Questions & discussion
- Pitfalls
- PDF of this chapter (or create customized PDF)
definition & diagnosis of hyperthermia
what is hyperthermia?
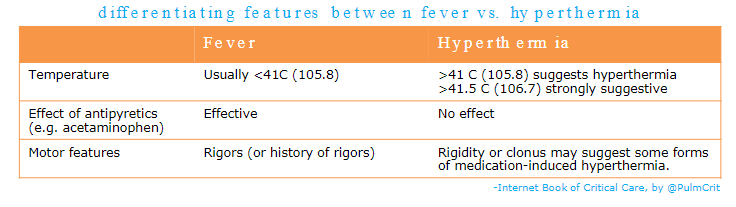
- Fever is temperature elevation due to activity of the hypothalamus, in response to cytokines. Such cytokines may be triggered by infection or sterile inflammation.
- Hyperthermia is temperature elevation due to uncontrolled heat generation (e.g. from muscular hyperactivity). This can generate higher temperatures than a fever, with a greater risk of thermal injury to tissues.
- Unlike fever, hyperthermia involves complete loss of thermal control.
heat stroke
heat stroke
- Disease caused by an imbalance of heat generation versus heat clearance from the body (without another primary underlying cause).
- Clinically defined on the basis of:
- (a) Temperature >40C (104F)
- (b) Neurologic manifestations (e.g. altered mental status, ataxia, seizure)
- (c) Caused primarily by exertion or exposure
exertional heat stroke
- Caused by exertion in hot weather (e.g. marathoners, military recruits).
- Diagnosis is generally reasonably obvious based on history.
- Patients can be sweaty.
non-exertional heat stroke
- Results from lack of adequate hydration and air conditioning during a heat wave.
- Usually affects elderly with medical comorbidities.
- Presentation may be less obvious than exertional heat stroke (should have high index of suspicion during a heat wave).
- Examination may show dry skin, delirium, and abnormal vital signs (e.g. hyperthermia, tachycardia, hypotension).
differential diagnosis
heat stroke (see above)
toxicologic
- Malignant hyperthermia
- Neuroleptic malignant syndrome
- Serotonin syndrome
- Sympathomimetic overdose
- Salicylate intoxication
- Anticholinergic intoxication
CNS disease
- Meningitis or encephalitis
- Hypothalamic disease (e.g. CVA or hemorrhage)
endocrinopathy
- Thyroid storm
- Pheochromocytoma
- Adrenal crisis
sepsis
- Usually doesn’t cause profound temperature elevation, but this can occur, especially in the following situations
- (a) CNS infection (meningitis/encephalitis)
- (b) Sepsis + other factors limiting heat loss (e.g. anticholinergics, phenothiazines)
evaluation
evaluation for organ damage
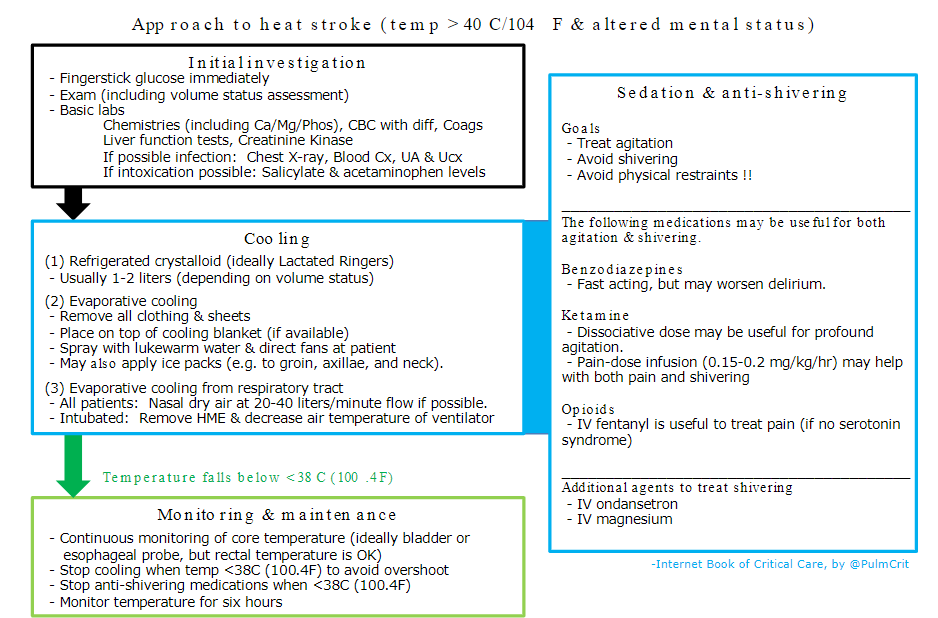
- Immediate fingerstick glucose if mental status alteration
- Chemistries, including Ca/Mg/Phos
- CBC with differential
- LFTs (hyperthermia can cause hepatic failure)
- Coags, fibrinogen, D-dimer (can cause DIC)
- Creatinine kinase (can cause rhabdomyolysis)
investigations to determine the etiology (if unclear)
- Review medications, changes in medications, and drug interactions (focusing on serotonergic medications)
- Cultures, lumbar puncture
- TSH, cortisol
- Neuroimaging (CT scan +/- MRI)
- If toxicologic cause is suspected
- Acetaminophen and salicylate levels
- Urine toxicologic screen may be considered
general supportive care
Some patients with hyperthermia have a causative problem that requires specific management (e.g. brainstem stroke, meningitis, septic shock). However, the most important aspect of care overall is usually meticulous and aggressive supportive care.
sedation & shivering treatment
role of sedation
- May be important, regardless of whether the patient is intubated.
- Ongoing agitation must be avoided:
- Muscular exertion may increase risk of rhabdomyolysis.
- Activity increases heat generation, impairing the ability to control hyperthermia.
- Never use physical restraints to control agitation (struggling against restraints will further increase heat generation).
potential options
- Benzodiazepines
- Especially useful in hyperthermia that is due to intoxication (e.g. sympathomimetics).
- Beneficial properties include muscle relaxation and anti-seizure effects.
- Ketamine
- May be useful for immediate control of profound agitation.
- Propofol
- Useful among intubated patients.
- Advantages include anti-seizure activity and the ability to lift sedation to re-evaluate mental status.
- Opioids
- Sources of pain should be treated appropriately (especially if these are drivers of agitation).
- If serotonin syndrome is possible, then fentanyl should be avoided.
- Dexmedetomidine
- Possible consideration for non-intubated patients, since it is titratable and doesn’t suppress respiration.
- Sympatholytic properties may assist with control of shivering.
- Logistically challenging to initiate rapidly (loading bolus should be avoided given potential for bradycardia).
suppression of shivering
- Shivering will impair temperature management and should be controlled during the acute cooling phase.
- For the intubated patient, paralysis with a non-depolarizing muscle relaxant may be used to control shivering (see below).
- For a patient who isn’t intubated, the following medications may be used (several may be needed)
- IV benzodiazepines and/or IV dexmedetomidine (depending on patient’s mental status reserve).
- Fentanyl (if there is no suspicion of serotonin syndrome).
- Pain-dose ketamine infusion has some anti-shivering properties (e.g. 0.15-0.3 mg/kg/hr).
- IV magnesium.
- Buspirone 30 mg enterally.
- IV ondansetron has some anti-shivering effects.
intubation if necessary
indications to consider intubation
- (1) Cause of hyperthermia is unclear and intubation will be required to achieve necessary diagnostic studies (e.g. lumbar puncture and MRI).
- When in doubt, an alternative approach is to cool the patient and determine if mental status normalizes. If temperature control normalizes mental status, this argues against meningitis or CVA.
- (2) Severe rigidity interferes with mechanical ventilation or temperature control (e.g. in extreme serotonin syndrome).
- (3) Status epilepticus
- Seizure can rapidly initiate a vicious cycle of worsening hyperthermia and intractable seizure leading to death.
- In any patient with hyperthermia and repeated or ongoing seizure, there should be a very strong consideration to immediately treat with propofol and ketamine (to control seizure) and subsequently intubate.
- (4) Other usual indications, such as:
- Worsening respiratory failure
- Refractory agitation
intubation procedure itself
- Avoid succinylcholine
- May confuse matters later regarding the possibility of malignant hyperthermia.
- May worsen hyperkalemia (which can occur in these patients).
- Continuation of paralysis for 1-2 hours after intubation may facilitate temperature control (e.g. perform rapid sequence intubation using rocuronium and then give 1-2 subsequent doses of vecuronium q30-45 minutes).
- Obviously, ensure that the patient is adequately sedated during this period.
- Paralysis will eliminate all heat generation by skeletal muscles, accelerating achievement of target temperature.
temperature control overview
monitoring
- Core temperature should ideally be monitored in real time, to prevent overshoot hypothermia.
- The best ways to achieve this are usually an esophageal probe (intubated patients) or a bladder probe (non-intubated patients).
- Rectal temperature may be monitored if nothing else is available, but this may tend to lag behind other modes of temperature measurement.
temperature goals
- #1) Initially, drop the core temperature to 38C (100.4F) as rapidly as possible.
- #2) Stop active cooling when the temperature falls below <38C or <100.4F (to prevent overshoot).
- #3) Continue monitoring for ongoing thermal instability (ideally at least for 6 hours).
multi-modal cooling
- The techniques below are intended to be initiated immediately and used simultaneously.
- Each technique removes thermal energy from the body. These techniques function in an additive fashion.
- The most important technique is surface cooling (#2 below) which is absolutely essential. Agressive surface cooling will work fine on its own. However, internal and respiratory cooling are useful adjunctive techniques which are easy and may help achieve target temperature faster.
(1) internal cooling: crystalloid
refrigerated crystalloid
- Ideally there should be a supply of pre-chilled IV fluid (e.g. bags of Lactated Ringers stored in a refrigerator).
- Each liter of chilled crystalloid will cool the patient by roughly ~1 degree Centigrade.
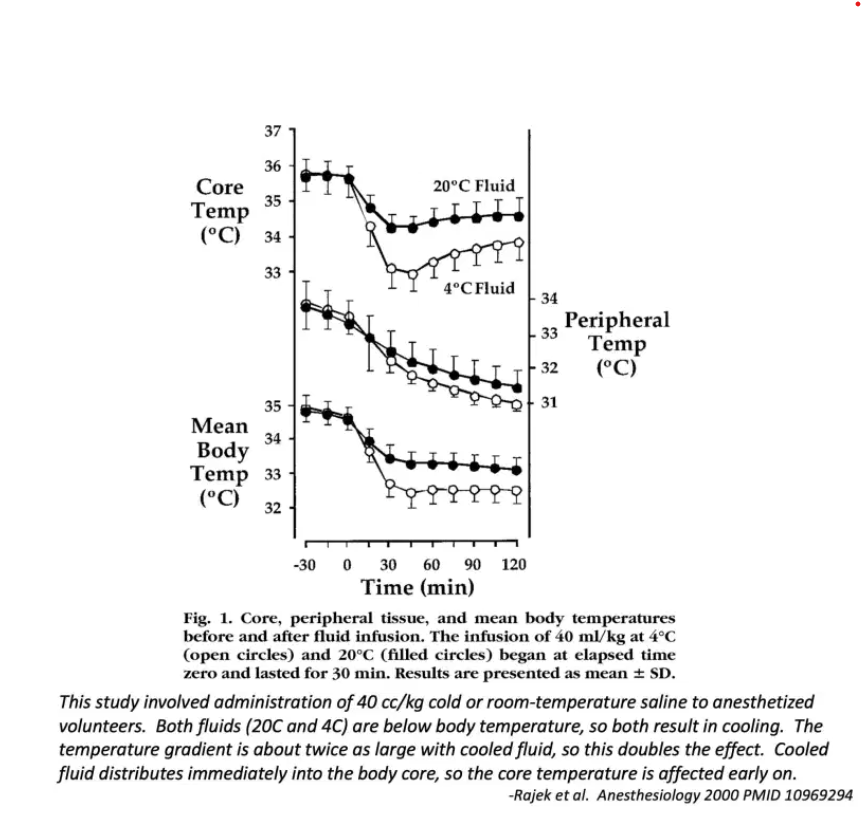
pharmacokinetics of thermal energy: cooled IV fluid directly affects the core temperature
- The body is sometimes modeled as a single vat of fluid which is constantly mixed together, thereby achieving a single temperature. This isn’t the way the body functions in real time, for example:
- A core temperature exists in the large blood vessels and organs receiving high levels of perfusion (e.g. heart, brain). This is more important with regards to target organ damage (especially brain injury).
- A peripheral temperature exists in tissues contacting the environment (e.g. skin and soft tissues).
- Surface cooling techniques involve removal of thermal energy from the skin, with the aim that cooler temperatures will eventually be transmitted to the core. This is generally very effective, but it may be delayed in shocked patients with peripheral vasoconstriction (which delays temperature exchange between the core and periphery).
- Infusion of cooled fluid directly impacts on the core temperature. This allows it to be immediately effective, regardless of the state of peripheral perfusion.
- In shocked patients, cooled fluid might even have a disproportionate effect on the core body tissues (which would be desirable).
why external fluid is effective for cooling, but not for warming
- One common point of confusion is the following:
- Infusion of warmed fluid is poorly effective for warming patients with hypothermia.
- Infusion of cooled fluid is moderately effective for cooling patients with hyperthermia
- Why? The effect of infused fluid depends on the temperature gradient between the body and the infused fluid.
- Hypothermia: The body is ~32C, warmed fluid is perhaps ~40 C, so the temperature gradient is ~8 C.
- Hyperthermia: The body is ~44C, cooled fluid is perhaps ~4 C, so the temperature gradient is ~40 C.
- Physiology works in our favor here: the hotter the patient is, the more effective the cooled fluid will be. Evidence regarding the efficacy of cooled fluids was mostly obtained in patients starting at a normal temperature, so cooled fluids might be a bit more effective in hyperthermia.
evidentiary basis for cooled fluids
- Cooled fluids haven’t been studied in hyperthermia. However, the physiology and efficacy of cooled crystalloid is well established in a variety of contexts (pre-hospital medicine, anesthesiology, and neuro-critical care).
- The use of cooled fluids is perhaps best studied for rapid induction of hypothermia following cardiac arrest. This is widely recommended and incorporated into post-cardiac arrest protocols.
- Numerous studies support the ability of chilled crystalloid (at 0-4 C) to reduce core body temperature by roughly ~1 C per liter (i.e. ~2 C drop following receipt of 30-40 cc/kg)(22371279, 10969294, 18312676, 23809038, 25348858, 15733765, 25563645, 12505732, 16352954). This is extremely well established at this point, for example it’s been validated in large prospective RCTs (24240712).
(2) surface cooling
Choice of physical cooling method depends on available resources and the cause of hyperthermia. The best options here are evaporative cooling or an ice bath.
remove all clothing
- Clothing impedes heat egress from the body.
- Regardless of which technique you’re using for cooling, clothing will work against you.
- Don’t cover patients with sheets – this will likewise impair cooling (especially with evaporative cooling).
(a) evaporative cooling
- Spray the unclothed patient with lukewarm water and direct a fan at them. If you don’t have a spray bottle, anything which generates fine water particles will work (e.g. mucosal atomizer device or similar equipment designed to deliver drugs to the airway or nose).
- Note that the water shouldn’t be cold (this will decrease the amount of evaporation).
- Evaporation is very effective at cooling the body (roughly ~0.1 C per minute).
- Add-ons:
- (1) Add a cooling blanket underneath the patient to maximize heat loss through the posterior body surface.
- (2) Ice packs may also be placed (e.g. on the groin, axillae, and neck).
- Conductive heat loss is faster than evaporative heat loss. These add-ons will therefore increase the rate of cooling. As more and more ice packs are added and the patient is covered in ice this approach will eventually start to resemble an immersive ice bath (below).
- Evaporation won’t work if the ambient humidity is high (e.g. >70%); this may fail in areas which aren’t dehumidified.
(b) immersive ice bath
- Most effective method of physical cooling (roughly ~0.2 C per minute)(31216400).
- The gold standard for rapid cooling is filling a bath of water with ice and allowing water in the bath to reach zero degrees centigrade prior to patient immersion (true ice water immersion). This is often set up near marathons in anticipation of exertional heat stroke and it’s insanely effective.
- Most hospitals don’t have this. Alternative techniques include the following:
- (a) Covering the patient in ice (see video below).
- (b) Placing the patient on a plastic sheet, covering the patient in ice, and then wrapping the sheets closed (“tarp taco” technique)(31221601).
- (c) Putting the patient in a body bag and filling the body bag with ice and water (credit this idea to @ToxAndHound).
Epic video on Bellevue’s Immersive Water Bath by Adaira Landry: [I couldn’t embed this video so definetely go to the chaper to watch it.]
(c) external pads with adaptive water-based cooling system (e.g., Arctic Sun)
- Eventually will work, but overall sluggish to get set up and running (may take the machine a while to cool down).
- This is not a preferred technique here, because the goal is decreasing the patient to target temperature in <30-60 minutes. The delay to set up external pads will make it difficult to meet this goal.
(3) respiratory cooling [See chapter section for the complete instructions]
caveats to this section
- (1) There isn’t much evidence supporting these interventions.
- (2) These techniques are intended only for short-term use (e.g. 1-3 hours) to help bring the patient’s temperature down from an immediately threatening level.
- (3) These techniques are solely adjunctive techniques (not intended as the primary technique for cooling).
management of complications
potential complications include:
- Rhabdomyolysis
- Acute hepatic failure (rarely leading to fulminant failure requiring transplantation)
- Seizure
- Aspiration pneumonia; ARDS
- Stress-induced cardiomyopathy, arrhythmia
- Disseminated intravascular coagulation (DIC)
- [Link is to IBCC chapter, Acute Disseminated Intravascular Coagulation (DIC)
December 5, 2016 by Dr. Josh Farkas]- Hypoglycemia
- Hyponatremia
These complications should be treated using standard supportive measures. Consider monitoring laboratory studies (especially creatinine kinase and liver function tests) over the first 24 hours to watch for the emergence of these problems.
summary
PITFALLS
- Failure to promptly cool hyperthermic patients, resulting in thermal organ damage.
- Use of non-core temperature measurements.
- If you’re going to use a respiratory cooling technique (e.g. removal of the ventilator heat and moisture exchanger), make sure to discontinue this after a few hours, once the patient has reached a safe temperature.
- There’s no role for acetaminophen or other antipyretic medications (hyperthermia isn’t mediated by the thalamus, so these medications will have no efficacy).
- Avoid the use of vasopressors if possible, as this may cause cutaneous vasoconstriction which impairs heat release.
Going further:
- Heat Stroke (Stuart Swadron and Bob Paquette, EM:RAP)
- Heat Stroke (WikiEM)
- Rhabdomyolysis & exertional heat stroke (Michelle O’Connor and Moira Carroll, emDocs)
- Hyperthermia Syndromes (Anand Swaminathan, RebelEM)