In addition to The Cribsiders #27 in this post, I include a section on Pediatric Advanced Life Support from p. 72 on compensated shock from the 2020 Handbook Of Emergency Cardiovascular Care For Healthcare Providers.
I also link to Anomalous Left Coronary Artery From the Pulmonary Artery
Updated: Aug 10, 2020. Author: Mary C Mancini, MD, PhD, MMM from emedicine.medscape.com.
And finally, I link to The Cribsiders‘ [Link is to the complete episode list] #5 MIS-C: When COVID Affects Kids AUGUST 12, 2020 By DR JUSTIN BERK.
In this post, I link to and excerpt from The Cribsiders‘ #27: Shock! A Deep Dive into Our First Intensive Topic. JUNE 9, 2021 By DR JUSTIN BERK.
All that follows is from the above outstanding podcast and show notes on pediatric shock.
Shock Pearls
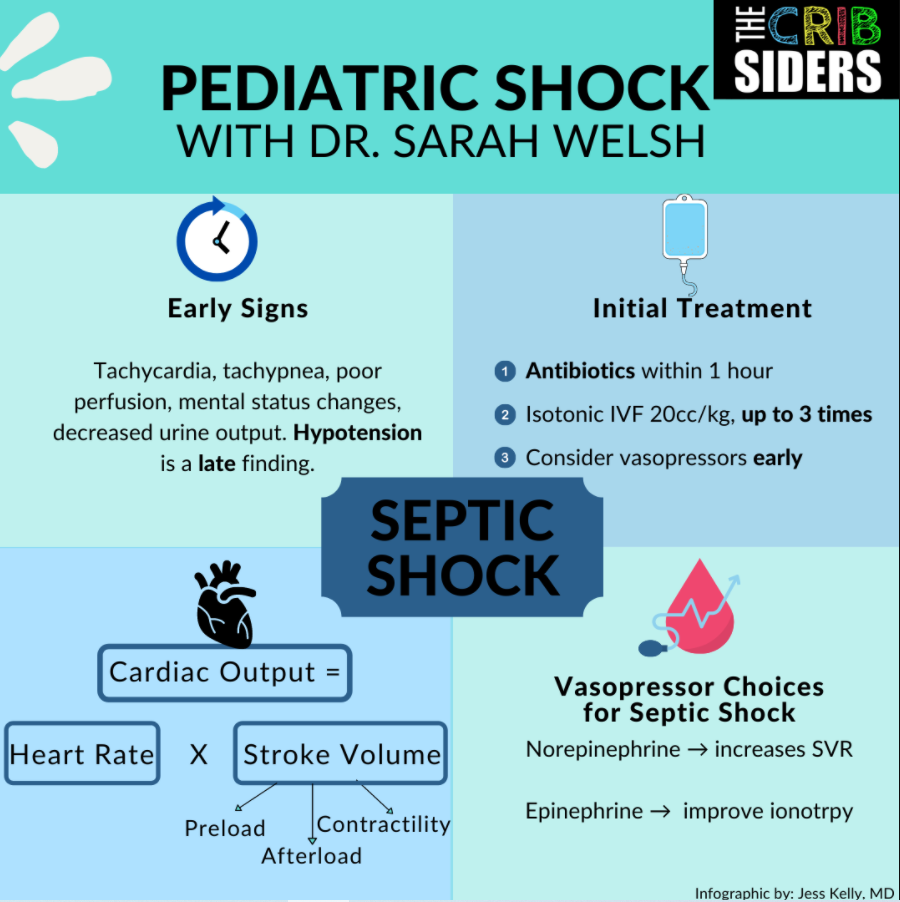
- Patients with septic shock should receive antibiotics within 1 hours of presentation and no more than 60cc/kg of isotonic fluids. Vasoactive medications such as norepinephrine and epinephrine and should be thought about early.
- Patients in cardiogenic shock can be worsened by IV fluids and should be treated with attempts to improve cardiac output by decreasing afterload and increasing contractility or lusitropy, such as with milrinone and dobutamine.
- Trauma patients with hemorrhagic shock may have bleeding into the abdomen, pelvis, or femur. They need a type and cross and may require a massive transfusion protocol and balanced transfusions.
- Neurogenic shock presents as hypotension, bradycardia, and peripheral vasodilation as the result of unopposed parasympathetic activity in the setting of a spinal cord injury.
- Steroids are not routinely used in shock, but steroids may be indicated in treating shock that is refractory to multiple pressors.
Pediatric Shock Notes
Dr. Welsch describes how shock can present in a variety of ways. She describes the many forms of shock including septic, cardiogenic, obstructive, hemorrhagic, neurogenic, and refractory shock.
Take Home Points
TACHYCARDIA IS AN EARLY WARNING SIGN FOR SHOCK. PAY ATTENTION TO THE NORMAL VITAL SIGNS FOR THE PATIENT’S AGE. THE NORMAL HEART RATE FOR 12-18 YEAR OLDS IS LESS THAN 100.
HYPOTENSION (UNCOMPENSATED SHOCK) IS A LATE FINDING IN SHOCK. COMPENSATED SHOCK* IS WHEN TACHYCARDIA OR VASCULAR RESISTANCE ARE INCREASED TO PREVENT HYPOTENSION.
STAY AT THE BEDSIDE AND CONTINUALLY REASSESS YOUR INTERVENTIONS FOR A PATIENT WITH SHOCK.
__________________________________________________________
*All that follows is from The 2020 Handbook Of Emergency Cardiovascular Care For Healthcare Providers, p. 76-Pediatric Advanced Life Support:
Initial Assessment
Primary cardiac arrest in children is much less common than in adults. Cardiac arrest in infants and children does not usually result from a primary cardiac cause; rather, it is the end result of progressive respiratory failure or shock. To prevent pediatric cardiac arrest, providers must detect and treat respiratory failure, respiratory arrest, and shock in a timely manner.
Conditions Indicating Need For Rapid Assessment and Potential Cardiopulmonary Support [Meaning Conditions Suggesting Compensated Shock]
- Irregular respirations or or reate greater than 60 breaths/min.
- Heart rate ranges (particularly if associated with poor perfusion)
- Child 2 years or younger: less than 80/min or greater than 180/min
- Child older than 2 years of age: less than 60/min or greater than 160/min
- Poor perfusion*, with weak or absent distal pulses
- *[Prolonged capillary refill. Signs of end organ failure {also] include altered mental status (poor oxygen delivery to the brain) and poor urine output.
- Increased work of breathing (retractions nasal flaring, grunting)
- Abnormal respirations (eg, bradypnea, seesaw breathing)
- Cyanosis or a decrease in oxyhemoglobin saturation
- Altered level of consciousness (unusual irritability or lethary or failure to respond to parents or painful procedures) [again, a sign of end-organ failure due to inadequate perfusion]
- Seizures
- Fever with petechiae
- Trauma
- Burns involving more than 10% of the body surface area
Vital Signs In Children
These 3 tables below are from Hanzinski M. Children are dfferent. In Nursing Care Of The Critically Ill Child. 3rd ed. Mosby: 2013:1-18. copyright Elsevier.
Normal Heart Rates*
Age Awake Rate (beats/min) Sleeping Rate (beats/ min Neonate 100-205 90-160 Infant 100-180 90-160 Toddler 98-140 80-120 Preschooler 80-120 65-100 School age child 75-118 58-90 Adolescent 60-100 50-90 *Always consider the patient’s normal range and clinical condition. Heart rate will normally increase with fever or stress.
Normal Respiratory Rates*
Age Rate (breaths/min) Infant 30-53 Toddler 22-37 Preschooler 20-28 School-age child 18-25 Adolescent 12-20 *Consider the child’s normal range. The child’s respiratory rate is expected to increasw in the presence of fever or stress. Data from Fleming S et al. Lancet. 2011;377(9770): 1o11-1018.
Normal Blood Pressures
Age Systolic Pressue (mm Hg)* Diastolic Pressure (mm Hg)* Mean Arterial Pressure (mm Hg)† Birth (12 h, < 1000 g) 39-59 16-36 28-42† Birth (12 h, 3 kg) 60-76 31-45 48-57 Neonate (96 h) 67-85 36-53 45-63 Infant (1-12 mo) 72-104 37-56 50-62 Toddler (1-2 y) 86-106 42-63 49-63 Preschooler (3-5 y) 89-112 46-72 58-69 School-age child (6-9 y) 97-119 57-76 66-72 Preadolesent (10-12 y) 102-120 61-90 71-39 Adolescent 110-131 64-83 73-84 *Systolic and dastolic blood pressure ranges assume 50th percentle for height children 1 year and older.
†Mean arterial pressures (diastolic pressure + [difference between systolic and diastolic pressures]/3) for 1 year and older, assuming 50th percentile for height.p formula (which I believe is a misprint) on p. 76 of the 2020 Handbook of Emergency Cardiovascular Care For Healthare Proiders¹. Reference 1 below has the correct formula. ]
‡Approximately equal to postconception age in weeks (may add 5 mm Hg)
________________________________________________________
Now resuming excerpts from The Cribsiders’ #27 Pediatric Shock
Septic Shock
PRESENTATION
Assess on physical exam for fever, tachycardia (increases cardiac output), tachypnea, perfusion, and mental status. Know the normal vital sign ranges from neonates to adults in order to know when (and how much) to be worried about abnormal vital signs like tachycardia.
Hypotension is an obvious but a late finding of shock in pediatrics because kids have robust hearts and compensatory mechanisms. Signs of end organ failure include altered mental status (poor oxygen delivery to the brain) and poor urine output.
THE SPECTRUM: SYSTEMIC INFLAMMATORY RESPONSE SYNDROME (SIRS) TO SHOCK
- SIRS is >2 of the following: hyper/hypothermia, tachycardia, bradycardia (if <1 year), tachypnea, or abnormal white blood cell count or bandemia.
- Sepsis: SIRS + an infectious source
- Severe Sepsis: Sepsis + end organ dysfunction
- Shock: Severe sepsis + not responding to initial resuscitation
INITIAL MANAGEMENT
Start with the ABCs. Make sure they are protecting their airway (may be altered and need to be intubated). Ensure adequate oxygenation. In septic shock, oxygen demand outstrips delivery.
Address circulation by starting with fluid resuscitation and thinking about pressors early. IVF will address preload problems (dehydration, poor PO intake). Fluids do not address all of the etiologies of shock.
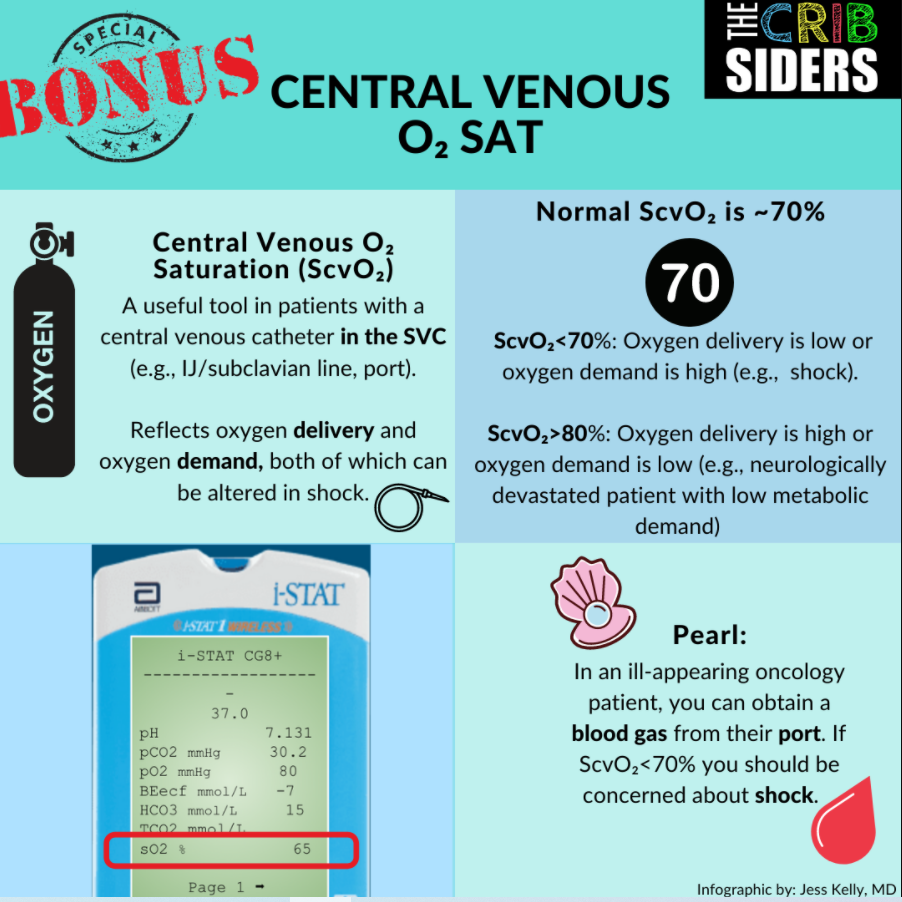
Obtain broad cultures (blood, urine, +/- CSF), CBC, CRP, electrolytes, CMP (transaminitis indicates end organ dysfunction), blood gas, lactate, and base deficit. The base deficit is a calculated value that helps tell you if there are additional acids in the blood (such as lactic acid or ketones). In sepsis, a more negative base deficit indicates that there is oxygen demand that is not being met and lactic acid is being produced. For more, check out this acid-base podcast by Dr. Scott Weingart.
Start targeted antibiotics within 1 hour of recognition of sepsis (Surviving Sepsis Campaign). Consider if your patient needs broader antibiotics (e.g., if they have fever + neutropenia).
IV FLUIDS
Surviving Sepsis Campaign recommends giving IVF boluses of 20cc/kg (each bolus up to max of AL 1L) up to 3 times and then strongly consider vasoactive medications if end organ evidence of shock persists.
The FEAST trial in Africa showed children who got more fluids in shock did worse. Consider smaller amounts if worried about cardiogenic shock and right heart failure. Give normal saline (NS), Lactated ringers (LR), or Plasma-lyte. Repeated NS boluses cause a hyperchloremic non-anion gap metabolic acidosis. Stay tuned for results from the The PRoMPT BOLUS study to see what is the best IVF to bolus with for children in septic shock. Re-assessment is key. Stay at the bedside and assess improvement of vital signs and an age-appropriate mean arterial pressure (MAP). Closely follow skin perfusion, urination, and mental status. Expert Opinion: Bedside ultrasound of inferior vena cava (IVC) diameter and IVC/aorta ratios may be helpful.
PRESSORS
Cardiac output = (Heart rate) x (Stroke Volume). Stroke volume components are preload, contractility/inotropy, and afterload.
The ideal pressor is specific to the patient. Pick a pressor based on what will best augment the patient’s cardiac output. Norepinephrine will increase systemic vascular resistance (increases preload). Epinephrine is used in children to help with sepsis-related myocardial dysfunction and inotropy issues.
Decreasing Metabolic Demand
Oxygen delivery = (oxygen content in the blood) x (cardiac output).
Think of oxygen delivery like getting a piece of mail: you need the mail in the system (arterial oxygen content) AND you need the mailman to deliver it (cardiac output). In sepsis, metabolic demand is outstripped by the body’s ability to deliver oxygen to tissues. Anything that can decrease demand is helpful. Antipyretics decrease fever and thus decrease metabolic demand. Intubation and sedation (even if not in respiratory failure) can also decrease metabolic demand.
Cardiogenic Shock
PRESENTATION
Cardiac dysfunction can present with poor perfusion/decreased pulses, hypotension, tachycardia, and hepatomegaly. Hepatomegaly can indicate elevated right sided pressures and right sided heart dysfunction.
CAUSES
Sepsis-related myocardial dysfunction, viral myocarditis, congenital heart disease, post-cardiac arrest, arrhythmias (prolonged SVT), anomalous left coronary artery from the pulmonary artery (ALCAPA)*.
*Anomalous Left Coronary Artery From the Pulmonary Artery
Updated: Aug 10, 2020. Author: Mary C Mancini, MD, PhD, MMM:The occurrence of ALCAPA is generally similar between males and females, and it is not considered an inheritable congenital cardiac defect.
The occurrence of ALCAPA is generally similar between males and females, and it is not considered an inheritable congenital cardiac defect.
Approximately 85% of patients present with clinical symptoms of congestive heart failure within the first 1-2 months of life. In unusual cases, the clinical presentation with symptoms of myocardial ischemia may be delayed into early childhood. Though rare, presentation in adults have been reported. [5, 6, 7, 8] Rarely, a patient may stabilize following infarction and present with mitral valve regurgitation later in childhood or even adulthood.
Inadequate myocardial perfusion likely causes significant chest pain and these symptoms of myocardial ischemia may be misinterpreted as routine infantile colic. [3]
Multisystem inflammatory syndrome in children (MIS-C)* is a newly recognized hyper-inflammatory condition that can present in cardiogenic shock. Consider it in children who had a COVID exposure 6-8 weeks prior. Can start with screening labs (CBC, CRP, and BMP) looking for high CRP, thrombocytopenia, leukopenia, and hyponatremia. If abnormal, consider obtaining other labs such as troponin, BNP, d-dimer, fibrinogen, and ferritin.
*See The Cribsiders‘ [Link is to the complete episode list] #5 MIS-C: When COVID Affects Kids AUGUST 12, 2020 By DR JUSTIN BERK
MANAGEMENT
If a patient has high right sided pressures, right sided heart failure, and hepatomegaly, increasing preload with IVF will worsen the clinical picture. Ensure adequate preload (kids may be dehydrated) but don’t overdo it.
Address inotropy and left ventricular support by decreasing afterload and increasing contractility to improve cardiac output. Dobutamine is used to help with contractility/inotropy and afterload reduction. Milrinone is also used to help with afterload reduction, contractility/inotropy, and lusitropy. Lusitropy is diastolic relaxation that allows the ventricle to fill.
Warm shock (bounding pulses, skin is warm, flash capillary refill) is classically septic shock.
Cold shock (poor pulses, delayed capillary refill) is classically thought of as cardiogenic shock.
Editor’s Note: Warm and cold shock are difficult to differentiate clinically. Warm shock is a type of shock seen in pediatrics, not adults. A good starting point is to treat warm shock with norepinephrine (need the alpha-agonist to help with vasoconstriction) versus cold shock with epinephrine (need the beta-agonist activity to help cardiac output).
Obstructive Shock
PRESENTATION
External compression of the heart causes the heart to be unable to deliver the cardiac output the body needs.
Desaturations, decreased breath sounds, and narrow pulse pressure in the trauma patient raises concern for tension pneumothorax, hemothorax, pericardial effusion, and pericardial tamponade. Editor’s note: A massive pulmonary embolism is another top cause of obstructive shock in children.
MANAGEMENT
Ultrasound can help to know if there is air or fluid present that is compressing the lungs or heart. To drain a pneumothorax or hemothorax, place a chest tube at the mid-axillary or mid-clavicular line, 4th-5th rib, above the rib to avoid neurovascular bundles.
Hemorrhagic Shock in the Trauma Patient
BLUNT ABDOMINAL ORGAN INJURY AND PELVIC OR FEMUR FRACTURES ARE PLACES FOR POTENTIAL BLOOD LOSS.
MANAGEMENT
In the trauma patient, start with ABCs. Obtain trauma labs such as type and screen, CBC, electrolytes, CMP, coags, d-dimer, fibrinogen. There are institution-specific massive transfusion protocols. Patients with hemorrhagic shock may need balanced transfusions of pRBCs, platelets, and plasma. Be sure to obtain appropriate imaging ASAP. May need a CT PAN scan (CT brain, chest, and abdomen/pelvis) depending on mental status and injuries.
Neurogenic Shock
THE TRIAD OF HYPOTENSION, BRADYCARDIA, AND PERIPHERAL VASODILATION IS SPINAL CORD INJURY. THE SPINAL CORD CAN BE TRANSECTED OR STUNNED WITH INJURY SUCH AS BEING UNRESTRAINED IN A MOTOR VEHICLE CRASH. THE SYMPATHETIC PATHWAYS ARE INJURED AND THERE IS UNOPPOSED PARASYMPATHETIC ACTION, WHICH IS DIFFICULT TO TREAT. START WITH EARLY INITIATION OF PRESSORS, EPINEPHRINE, ATROPINE, OR ISOPROTERENOL.
Adrenal Crisis
WHEN A PATIENT IS REFRACTORY TO THERAPY, CONSIDER ADRENAL INSUFFICIENCY, ESPECIALLY IN PATIENTS WHO HAVE RECEIVED REPEATED STEROID COURSES IN THE SETTING OF A RECENT STRESS SUCH AS SURGERY. HYPERKALEMIA AND HYPONATREMIA ARE OFTEN PRESENT. HYDROCORTISONE DOSE IS USUALLY 100MG/M2. POST-CARDIAC ARREST CAN CAUSE ADRENAL INSUFFICIENCY. PREVIOUSLY HEALTHY KIDS PRESENTING IN SHOCK USUALLY DO NOT HAVE ADRENAL INSUFFICIENCY. THE SURVIVING SEPSIS CAMPAIGN RECOMMENDS STEROIDS WHEN TREATING SHOCK THAT IS REFRACTORY TO MULTIPLE PRESSORS.
REMEMBER FROM MED SCHOOL WATERHOUSE–FRIDERICHSEN SYNDROME, OR BLEEDING INTO THE ADRENAL GLANDS IN THE SETTING OF BACTERIAL INFECTION SUCH AS NEISSERIA MENINGITIDIS.
Post-op Patients
ALWAYS REMEMBER ANESTHESIA AND SEDATION MEDICATIONS CAN DROP YOUR SYSTEMIC VASCULAR RESISTANCE AND FLUIDS WILL NOT WORK EFFECTIVELY TO FIX THEIR BLOOD PRESSURE.
Links
- OPENPediatrics: Freely available modules for many topics in pediatrics including shock.
- Society for Critical Care Medicine: A great website with lots of resources
- Pediatric Critical Care Medicine: A great journal for critical care topics.