Children and adults who are on a ketogenic diet require careful and thorough evaluation when they exhibit acute illness. Please see clinical guideline Ketogenic diet acute illness management from The Royal Children’s Hospital Melbourne. Although the guideline is for children, the same management principles would apply for adults.
Matthew’s Friends: Ketogenic Dietary Therapies is a British website that is similar to the Charlie Foundation. And it also has many excellent resources on ketogenic diet therapy.
The Charlie Foundation For Ketogenic Therapies was founded in 1994 and here are some excerpts from the About Us page:
The Charlie Foundation for Ketogenic Therapies was founded in 1994 to provide information about diet therapies for people with epilepsy, other neurological disorders and select cancers. Charlie Abrahams, pictured above, continues to be the inspiration for the foundation, working as a pre-school teacher, and proving that Epilepsy can be cured through Ketogenic Therapy.
New applications of the Ketogenic Diet for cancer, autism, ALS, Parkinson’s Disease, type-2 diabetes, and traumatic brain injury have emerged. . . . To this end we have re-named ourselves “The Charlie Foundation for Ketogenic Therapies”.
Background On The Ketogenic Diet
What Are The Benefits Of Ketosis
Achieving a state of ketosis can have many benefits from treating chronic illnesses to optimizing performance. While the benefits are well documented, the underlying mechanism of action is not entirely known. The diet seems to enhance the ability of mitochondria, the power plants of our cells, to deliver our bodies’ energy needs in a manner that reduces inflammation and oxidative stress. Through optimizing the way our body uses energy, we fortify our bodies’ ability to take on the ever-growing stressors of our modern way of living.
How Do I Get Into Ketosis
There are two methods to make the metabolic shift from using glucose to ketones as your main source of energy.
The following are excerpts from Keto Therapies and from the individual therapy pages from The Charlie Foundation For Ketogenic Therapies.
The Five Variation Of The Ketogenic Diet
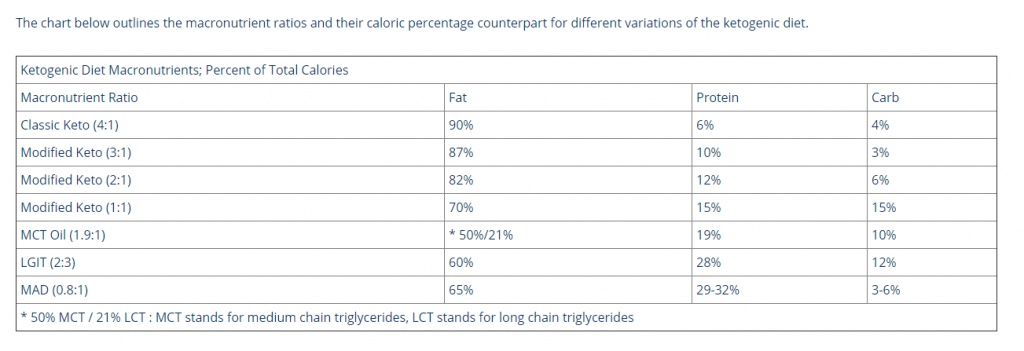
There are five variations of the Ketogenic Diet which have been published in medical literature as effective treatments for diseases that have an underlying metabolic dysregulation, such as epilepsy, cancer, and Alzheimer’s.
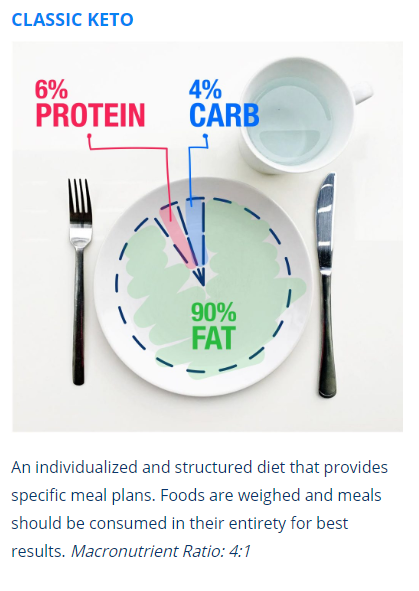
“The classic KD is calculated in a ratio of grams of fat to grams of protein plus carbohydrate combined. The most common ratio is 4 g of fat to 1 g of protein plus carbohydrate (described as “4:1”); 90% of calories are from fat. A 3:1 or lower ratio can be used alternatively to increase protein or carbohydrate intake; this is more appropriate as well for diet initiation in infants. There is one publication reportingthat a 4:1 ratio, when used at initiation, may be moreadvantageous for the first 3 months in older children, after
which the ratio can be reduced.85″*
*The above quote is from Resource (2).
The Classic Ketogenic Diet is the original Ketogenic Diet that was designed in 1923 by Dr. Russell Wilder at the Mayo Clinic for the treatment of epilepsy. With a 4:1 ratio of fat to protein and carbs, 90% of calories come from fat, 6% from protein, and 4% from carb. Although a 4:1 ratio is considered the gold-standard for classic Keto, a 3:1 ratio is also included in descriptions of classic KD in most publications. Notwithstanding, classic Keto is an individualized and structured diet that provides specific meal plans. Foods are weighed and meals should be consumed in their entirety for best results. The ratio of this diet can be increased for a more therapeutic outcome, and also liberalized for better tolerance. This diet is also considered a low glycemic therapy and results in steady glucose and insulin levels.
The Modified Ketogenic Diet
The Modified Ketogenic Diet is a less restrictive version of classic Keto, and can be helpful when starting the diet, or when tapering down to a less restrictive, long term diet. Carrying a macronutrient ratio between 2:1 -1:1, the diet is designed with flexibility in mind to increase compliance and decrease potential digestive discomfort and nutrient deficiency that can occur with long term classic keto eating.
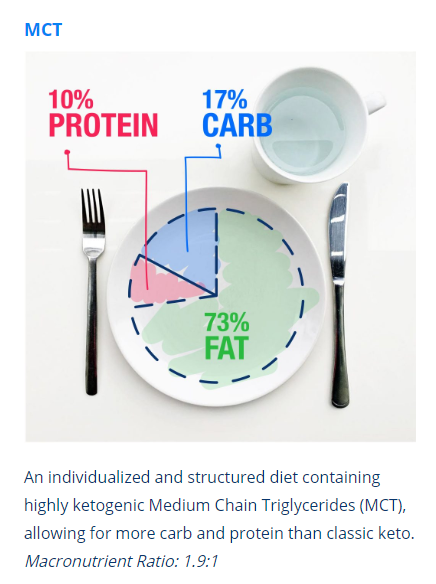
The Medium-Chain Triglyceride (MCT) oil diet is a less restrictive approach to the Ketogenic Diet. It is often used in England and Canada, though seldom used in the United States. The MCT oil diet is more flexible and allows a larger variety of food can be included due to the higher carbohydrate and protein allowance (macronutrient Ratio is 1.9:1). Medium-chain triglycerides produce ketones more easily than long-chain triglyceride (LCT) fat, with certain MCTs bypassing the liver and converting directly into ketones. This means that less total fat is needed, allowing more carbohydrate and protein to be included in the regimen.
Exchange lists divide up the allocated food groups for the day, giving the flexibility of planning individually designed meals by choosing from the lists in measured quantities. Experience has shown that better ketone levels are reached and tolerance obtained if the MCT oil is divided up evenly across the day between both snacks and meals. In other words, all food must be accompanied by a proportion of MCT.
Coconut oil is the most common source of MCTs. There are specialized formulations available that divide coconut oil into separate fatty acids. An explanation of the four types of MCTs will clarify which may be beneficial for you. MCTs differ by the number of their carbon bonds. Caprylic acid, for instance, has 8 carbon bonds, and is abbreviated as C8. Some practitioners may advise using a combination of oils for example, using coconut oil and a C-8 oil is a common practice.
Caproic Acid (C6)
The shortest of the MCTs, this oil may cause a burning sensation in the back of your throat while consuming, as well as cause gastrointestinal distress, though is highly ketogenic. For this reason, C6 is generally filtered out of MCT oils.Caprylic Acid (C8)
Requiring only a three-step conversion process into cellular energy called ATP (compared to sugar’s 26), C8 is the fastest MCT to metabolize in the brain. C8 is the most ketogenic MCT, and, promotes gut health through its anti-microbial attributes. Its typically the most expensive of the MCT oils.Capric Acid (C10)
Similarly ketogenic as compared to C8, C10 carries a slower conversion rate into cellular energy.Lauric Acid (C12)
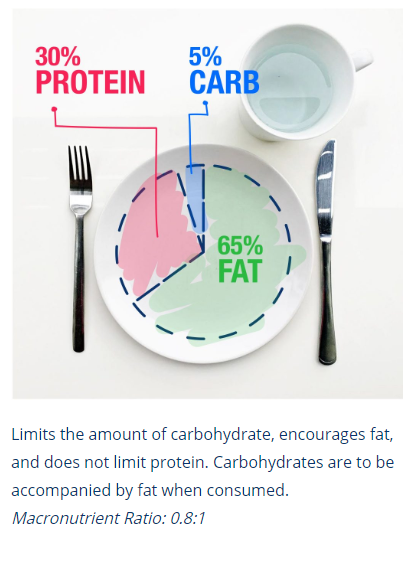
While technically considered an MCT, C12 acts more like an LCT biologically, requiring liver processing before being converted into useful energy. C12 has health benefits for the gut similar to C8 and C10.The Modifed Atkins diet (MAD) is a mix between the classic Ketogenic Diet, and the Atkins diet. The Atkins diet was created by a physician at John Hopkins named Dr. Robert C. Atkins in 1972, and limits carbohydrates while allowing for as much protein as the eater desires. The MAD, on the other hand, discourages too much protein, encouraging fat in its place. Carrying approximately a 1:1 macronutrient ratio, weighing of food is not required, and, total carbs per day is generally limited to 10-20 grams. It is important to read ingredient listings carefully to understand if there are carbs present despite what the nutrition facts panel reads. Unlike more restrictive Ketogenic Diets, MAD is usually initiated in an outpatient setting, though the person must still be monitored to ensure safety. The MAD is often used as a transition onto or from a more strict Ketogenic Diet, as well as for families lacking resources necessary to administer a more restrictive Keto plan.
The original Atkins diet is a very low in carbohydrate and was developed as a weight reduction therapy. The term “modified” describes the lower carbohydrate limit compared to Atkins recommendations and the emphasis of high fat foods as is required on the Ketogenic Diet.
The Low Glycemic Index Treatment (LGIT) is a diet that emphasizes complex carbohydrates over simple sugars, and is not intended to promote ketosis. Developed in 2002 as an alternative to the Ketogenic Diet, the LGIT constricts both the total amount of daily carbs and the Glycemic Index, referring to the effect on blood glucose after eating. As a general rule, the rate at which a particular food is digested and absorbed affects its glycemic index – so adding oil to a high carb meal reduces its glycemic index. The LGIT allows for an increased intake of carbohydrates versus a more strict Ketogenic Diet. Meals are based on portion sizes rather than measurement, allowing for a more flexible lifestyle. A booklet written by Massachusetts General Hospital for Children, explaining the LGIT, is available in our online store, and includes food lists, recipes, and tips.
The LGIT is a special high fat diet similar to the Ketogenic Diet that is used for difficult to treat seizures. It focuses on both the type of carbohydrate, low glycemic index, as well as the amount of carbohydrate based on portion sizes and household measurements. The glycemic index (GI) is a measure of the effect of carbohydrates on blood sugar levels. When carbohydrates are digested, they release glucose into the bloodstream. Carbohydrates that digest rapidly have a high GI. Carbohydrates that are digested slowly have a low GI. Foods are rated based on their GI values ranging from zero to 100. The LGIT includes foods that have a GI of 50 or lower. In addition to the GI, the digestion of a carbohydrate food is slowed by foods that are eaten at the same time that contain either fat or fiber. Therefore, meals are balanced with sources of fat, protein and a low glycemic index carbohydrate.
The Ketogenic Diets changes how the body uses energy. The diet provides ample fat which converts into fatty acids and ketones in the liver. This metabolic state is called ketosis, and, is the hallmark of the diet. Ketosis can also be achieved by fasting; both intermittent and prolonged periods without food. While the term ‘fasting’ is used to describe restrictive eating, fasting in this context is defined as a complete restriction of macronutrients long enough to deplete dietary energy and turn to the body’s energy stores of fat. Water must be consumed during fasting in sufficient amounts to help clear toxins from the body.
In order to understand how fasting works, it is helpful to review the ways in which the body stores energy. When food is not available to supply current energy needs, the body turns to its stored energy, either in the form of glycogen or fat. Glycogen consists of long chains of glucose derived from carbs which the body stores in the muscle and liver when we overeat carb. For example, if one were to eat a bowl of pasta that contains 500 carb-derived calories, the body’s breaks down these carbs into glucose. If the body only needs 200 calories worth of glucose to meet its immediate energy needs, 300 calories of glucose are stored in the form of glycogen for later use. The adult body can store, on average, 1,500 calories of glycogen in the muscles, and 500 in the liver. Once the body’s glycogen stores have been filled, any excess glucose in the blood is stored as fat. Fat storage occurs when you overeat. There is no upper limit to how much fat a person can store, and it can be stored virtually anywhere in the body. As we look at the two forms of storage side by side, the body preferentially burns glycogen over fat; once glycogen has been depleted, the body turns to fat. As such, one cannot achieve a state of ketosis if his or her body has stored glycogen, as glucose will be produced from stored glycogen.
Fasting For Ketosis
As stated above, when macronutrients are completely restricted, the body sources energy from its own stores. Glycogen gets burned first, then fat. If one is following a typical western diet, where the majority of calories are coming from carb-centric meals per day, a fasted state is rarely achieved, and glycogen levels are rarely depleted. As such, the body seldom, if ever, switches to a fat-utilizing mode, and is therefore not efficient at burning fat for fuel. Moreover, the presence of insulin, a hormone that transfers glucose from blood to cells, is triggered by the consumption of carbs. This prevents lipolysis, which is the breakdown of body fat into useful energy. Being completely dependent on glucose to maintain optimal energy levels requires frequent feedings, and our hunger/satiety hormones ensure these needs are met. These hunger hormones are called Leptin and Ghrelin; Leptin signals satiety, and its release decreases an individual’s appetite. Ghrelin, on the other hand, signals hunger, increasing and individual’s appetite. A high carb diet is thought to increase levels of Ghrelin in relation to Leptin, while a fasting or a Ketogenic Diet seems to balance this signaling system.
The act of fasting shifts the body into a fat-burning mode. Fasting forces the body to first use stored glycogen, followed by fat for energy. Similar to a Ketogenic Diet, fat is being broken down into fatty acids and ketones, a state of ketosis is achieved. If one’s glycogen reserves are filled to capacity, it can take between 2-4 days of fasting to achieve ketosis. This prolonged fasting period can be difficult both physically and mentally. You should consult a medical professional prior to attempting a fast of greater than 24 hours without food. Prolonged fasting has been utilized for thousands of years, dating back to Hippocrates era, for the treatment of epilepsy. Since prolonged fasting is not sustainable over the long term, another form of fasting has been developed that offers a similar metabolic transition, called intermittent fasting. Simply put, intermittent fasting reduces the window of time one eats during the day. A typical eating window for someone practicing intermittent fasting is between 6-12 hours, compared to 16-18 hours for someone practicing a typical western style of eating. When the eating window is shortened, the body is forced to access stored energy more often. When coupled with a Ketogenic Diet, intermittent fasting can optimize levels of ketosis, as well as reduce the time it takes for the individual to become efficient at utilizing fat as their main source of fuel. An important added benefit of fasting is that it can improve the health of our gastrointestinal tract.
There are two methods to make the metabolic shift from using glucose to ketones as your main source of energy.
Fasting – the method of complete cessation of caloric intake for a prolonged period of time has been used to treat disease as far back as 400 B.C. when Hippocrates, the Father of Modern Medicine, employed the method for a myriad of ailments. Though this should be done under medical supervision,fasting is a safe, effective (and, some would say, the easiest) way to get into ketosis, quickly. For the average adult, a 48-hour fast will generally result in ketosis. After this fast, adopting a Ketogenic Diet will allow you to stay in ketosis. We recommend starting the fast at least 3 hours before bedtime on the first day, and eating at the same time 2 days later. While fasting means many things to many people, we define it here as the total restriction of macronutrients. We recommend boosting water consumption in order to avoid dehydration, and many find black coffee or plain tea to help maintain focus and performance during the fast. Children go into ketosis much faster and therefore can be started on the diet without fasting and should also have close medical monitoring.
Diet – adopting a high fat, moderate protein, and low net-carb diet, will result in ketosis, and will take 2-3 weeks to achieve a consistent state, as defined above. We will go into diet options below, but you can also link to them here. During this period of transition, one can experience flu-like symptoms and tiredness. There can also be emotional unease related to longing for high-carb foods. Working with an experienced Ketogenic Specialist can help to minimize these effects.
Additional Resources:
(1) Ketogenic Diet: Which Patients Benefit? from Medscape
John Watson; Reviewed by: Anya Romanowski, MS, RD DISCLOSURES March 20, 2018
(2) Optimal clinical management of children receiving dietary therapies for epilepsy: Updated recommendations of the International Ketogenic Diet Study Group [Pubmed Abstract] [Full Text HTML] [Full Text PDF]. Epilepsia Open. 2018 May 21;3(2):175-192. doi: 10.1002/epi4.12225. eCollection 2018 Jun.